
[ad_1]
London (CNN) – As countries remain frozen in confinement and billions of people lose their livelihoods, the numbers are pushing for a change that would mark the end of the coronavirus pandemic: a vaccine.
But there is another possibility, the worst case scenario: that no vaccine is ever developed. In this result, people’s hopes repeatedly rise and then fade, as various proposed solutions fall before the final hurdle.
Instead of eradicating covid-19, societies could learn to live with it. Cities would slowly open up and some freedoms would be returned, but on a short leash, if experts’ recommendations were followed. Testing and physical tracing will become part of our lives in the short term, but in many countries, abrupt self-isolation instruction could come at any time. Treatments can be developed, but outbreaks of the disease could still occur each year, and the global death toll would continue to rise.
It is a path rarely publicly supported by politicians, who speak optimistically about human trials already underway to find a vaccine. But many experts take that possibility very seriously, because it has happened before. Repeatedly.
LOOK: Girl asks Dr. López-Gatell an innocent question: If soap kills the coronavirus, why are there no soap vaccines?
“There are some viruses we still don’t have vaccines against,” says Dr. David Nabarro, professor of global health at Imperial College London, who also serves as special envoy to the World Health Organization for covid-19. “We cannot absolutely assume that a vaccine will appear, or that if it appears it will pass all efficacy and safety tests.”
“It is absolutely essential that all societies everywhere put themselves in a position where they are able to defend themselves against the coronavirus as a constant threat and to be able to live social life and economic activity with the virus in our midst,” he said. Nabarro to CNN.
Most experts remain confident that a covid-19 vaccine will eventually be developed, in part because, unlike previous diseases like HIV and malaria, the coronavirus does not mutate rapidly.
Many, including the director of the National Institute of Allergy and Infectious Diseases, Dr. Anthony Fauci, suggest that it could occur in a year or 18 months. Other figures, such as England medical director Chris Whitty, have rushed to the far end of the spectrum, suggesting that a year may be too soon.
But even if a vaccine is developed, making it happen on any of those deadlines would be a feat never before accomplished.
“We have never accelerated a vaccine to one year or 18 months,” Dr. Peter Hotez, dean of the National School of Tropical Medicine at Baylor College of Medicine in Houston, told CNN. “It doesn’t mean it’s impossible, but it will be a heroic achievement.”
“We need Plan A and Plan B,” he says.
When vaccines don’t work
In 1984, the then US Secretary of Health and Human Services. The US, Margaret Heckler, announced at a press conference in Washington that scientists had successfully identified the virus, which later became known as HIV, and predicted that a preventive vaccine would be ready to be tested in two years.
Almost four decades and 32 million deaths later, the world is still waiting for an HIV vaccine.
LOOK: Experimental HIV vaccine fails in South Africa
Instead of a breakthrough, Heckler’s claim was followed by the loss of much of a generation of gay men and the painful rejection of his community in Western countries. For many years, a positive diagnosis was not just a death sentence; He claimed that a person would spend his final months abandoned by their communities, while doctors debated in medical journals whether it was worth saving HIV patients.
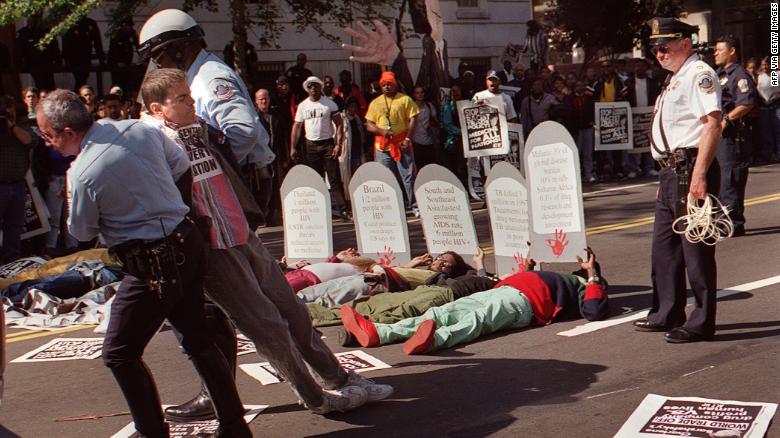
Protester Mark Milano is arrested during an AIDS protest in Washington in 1994.
The search did not end in the 1980s. In 1997 President Bill Clinton challenged the United States to invent a vaccine in a decade. Fourteen years ago, scientists said that we were still about 10 years away.
Difficulties in finding a vaccine started with the very nature of HIV / AIDS. “Influenza can change from one year to the next so that the natural infection or immunization from the previous year does not infect you the following year. HIV does so during a single infection, ”explains Paul Offit, a pediatrician and infectious disease specialist who co-invented the rotavirus vaccine.
“It continues to mutate in you, so it’s like you’re infected with a thousand different strands of HIV,” Offit tells CNN. “(And) while it’s mutating, it’s also paralyzing your immune system.”
HIV poses very unique difficulties and covid-19 does not possess its level of evasion, making experts generally more optimistic about finding a vaccine.
But there have been other diseases that have confused both scientists and the human body. According to the WHO, an effective dengue vaccine, which infects about 400,000 people a year, has eluded doctors for decades. In 2017, a large-scale effort to find one was suspended after the disease’s symptoms worsened.
LOOK: Dengue worries more and more in Latin America: what are its symptoms
Similarly, it has been very difficult to develop vaccines for common rhinoviruses and adenoviruses, which, like coronaviruses, can cause cold symptoms. There is only one vaccine to prevent two strains of adenovirus, and it is not commercially available.
“You have high hopes, and then your hopes are dashed,” says Nabarro, describing the slow and painful process of developing a vaccine. “We are dealing with biological systems, we are not dealing with mechanical systems. It really depends a lot on how the body reacts. “
Human trials are already underway at the University of Oxford in England for a coronavirus vaccine made from a chimpanzee virus, and in the USA. USA for a different vaccine, produced by Moderna.
However, it is the testing process, not development, that stops and often prevents the production of vaccines, adds Hotez, who worked on a vaccine to protect against SARS. “The difficult thing is showing that you can demonstrate that it works and that it is safe.”
Plan B
If the same fate happens to a covid-19 vaccine, the virus could stay with us for many years. But the medical response to HIV / AIDS still provides a framework for living with a disease that we cannot eliminate.
“With HIV, we have been able to turn that into a chronic disease with antivirals. We have done what we have always hoped to do with cancer, ”says Offit. “It is not the death sentence that it was in the 1980s.”
The innovative development of a daily preventive pill (pre-exposure prophylaxis, or PrEP) has led hundreds of thousands of people at risk of contracting HIV to be protected from the disease.
Various treatments for covid-19 are also being tested, as scientists are looking for a plan B in parallel to ongoing vaccine trials, but all of those trials are in very early stages. Scientists are analyzing remdesivir, an experimental drug against Ebola, while treatments with blood plasma are also being explored. Hydroxychloroquine, promoted as a potential “tipping point” by United States President Donald Trump, was found not to work in very sick patients.
“The drugs they have chosen are the best candidates,” says Keith Neal, professor emeritus of Epidemiology of Infectious Diseases at the University of Nottingham. The problem, he says, has been the “gradual approach” to testing them.

Remdesivir is one of the drugs tested to treat covid-19.
“We have to do randomized controlled trials. It’s ridiculous that we’ve only recently taken off, ”Neal, who reviews such evidence for inclusion in medical journals, told CNN. “The documents that I am seeing, I am simply rejecting them because they are not well done.”
Now those more comprehensive trials are ready, and if one of those drugs works for covid-19, the signs should appear “in a few weeks,” says Neal. The first may already have arrived; the US Food and Drug Administration. USA The FDA told CNN that it is in talks to make remdesivir available to patients after testing positive, which could accelerate recovery from the coronavirus.
The repercussions of successful treatment would be widely felt; if a drug can decrease the average time a patient spends in the ICU, even for a few days, it would free up hospital capacity and, therefore, could greatly increase the willingness of governments to open up society.
But how effective a treatment is will depend on which one works: remdesivir does not have a high international supply and increasing its production could cause problems.
LOOK: Remdesivir, a new drug authorized in the United States against covid-19
And, most importantly, any treatment will not prevent infections from occurring in society, which means that the coronavirus would be easier to manage and the pandemic would decrease, but the disease could be with us for many years.
What life looks like without a vaccine
If a vaccine cannot be produced, life will not remain as it is now. It may not return to normal quickly.
“Confinement is not economically sustainable, and possibly not politically sustainable,” says Neal. “So we need other things to control it.”
That means that as countries begin to come out of paralysis, experts will pressure governments to implement a new way of living and interacting to save time in the months, years, or decades until covid-19 can be eliminated. for a vaccine.
“It is absolutely essential to work to be prepared for covid,” says Nabarro. Calls for a new “social contract” in which citizens of all countries, as they begin to lead normal lives, take personal responsibility for isolating themselves if they show symptoms or come into contact with a possible case of covid-19.

Social estrangement and confinement could return until a vaccine is found.
It means that the culture of shaking off cough or light cold symptoms and going to work should be over. Experts also predict a permanent change in attitudes to remote work, with working from home for at least a few days, becoming a standard way of life for desktop employees. Companies would be expected to change their rotations so offices never fill up unnecessarily.
LOOK: The challenge of social distancing Cuba, where the lines are day by day
“(It should) become a way of behaving that we all attribute to personal responsibility … treating those who are isolated as heroes instead of pariahs,” says Nabarro. “A collective pact for survival and well-being against the threat of the virus.”
“It will be difficult to do in the poorest nations,” he adds, so finding ways to support developing countries will be “particularly difficult politically, but also very important.” He cites the tightly packed refugee and migrant settlements as areas of particular concern.
In the short term, Nabarro says that a comprehensive testing and contact tracing program would need to be implemented to allow life to work alongside covid-19 – one that overshadows any such program that has been established to combat an outbreak, and that It still seems far away in countries like the US. USA and the United Kingdom.
“Absolutely critical will be having a public health system that includes follow-up of contacts, diagnosis in the workplace, syndromic surveillance monitoring, early communication on whether we need to re-implement social distancing,” adds Hotez. “It’s doable, but it’s complicated and we really haven’t done it before.”
Those systems could allow some social interactions to return. “If there is a minimal broadcast, it is actually possible to open for sporting events” and other large gatherings, says Hotez, but that move would not be permanent and would be continually evaluated by governments and public health agencies.
That means the Premier League, NFL, and other massive events could go ahead with their schedules as long as athletes test regularly and fans are welcomed for weeks, perhaps separated within the stands, before quickly closing the stadiums if the threat increases.
“Bars and pubs are probably also last on the list, because they are overcrowded,” suggests Neal. “They could reopen as restaurants, with social distancing.” Some European countries have signaled that they will begin to allow restaurants to serve customers in very small capacity.
The restrictions are more likely to return during the winter, and Hotez suggests that spikes in covid-19 could occur every winter until a vaccine is introduced.
And the confinements, many of which are in the process of gradually being lifted, could return at any time. “From time to time there will be outbreaks, movement will be restricted, and that can apply to parts of a country, or even apply to an entire country,” says Nabarro.
READ: Fauci warns of the dangers of “skipping” the guidelines to overcome the coronavirus and the reopening of some states
The more time passes, the more compelling the prospect of community immunity becomes, achieved when the majority of a given population, about 70% to 90%, becomes immune to an infectious disease. “That to some extent limits the spread,” says Offit, “although population immunity caused by a natural infection is not the best way to provide population immunity. The best way is with a vaccine. “
Measles is the “perfect example,” says Offit, before vaccines became widespread, “2 to 3 million people get measles every year, and that would be true here, too.” In other words, the amount of death and suffering from covid-19 would be enormous, even if a large part of the population is not susceptible.
All of these predictions are tempered by the general belief that a vaccine will eventually be developed. “I think there will be a vaccine: there is a lot of money, there is a lot of interest and the objective is clear,” says Offit.
But if past outbreaks have proven anything, it’s that the search for vaccines is unpredictable. “I don’t think any vaccine has developed rapidly,” says Offit. “I would be very surprised if we had something in 18 months.”