[ad_1]
The way in which SARS-CoV-2 attacks a cell was detected by a team of infectious diseases from the Oswaldo Cruz Institute (IOC / Fiocruz). The images give a face to the virus responsible for the pandemic that affected 1.58 million people, killed 95,000 infected and locked more than a third of the planet’s population in their home.
The images, made by transmission electron microscope, were recorded in the study that seeks to know how Sars-CoV-2 replicates in the human body. The research identified the times when the virus invades and infects healthy cells.
Take advantage of their beaks (structure like the tips of a crown – crown in Latin, hence its name) to join the cell membrane, in a system known as “key and lock.” You already know that you prefer a specific block: the ACE2 receptor, used by the protein angiotensin-2 enzyme, which lowers blood pressure.
Devoured from the inside out
“When the virus recognizes ACE2, it binds to it and enters the cell, where it uses everything the cell has to reproduce. When it is just an empty shell, the virus breaks through the membrane and escapes, infecting the body with thousands of copies yours, “Oxford University professor of immunology Sarah Gilbert explained to the BBC.
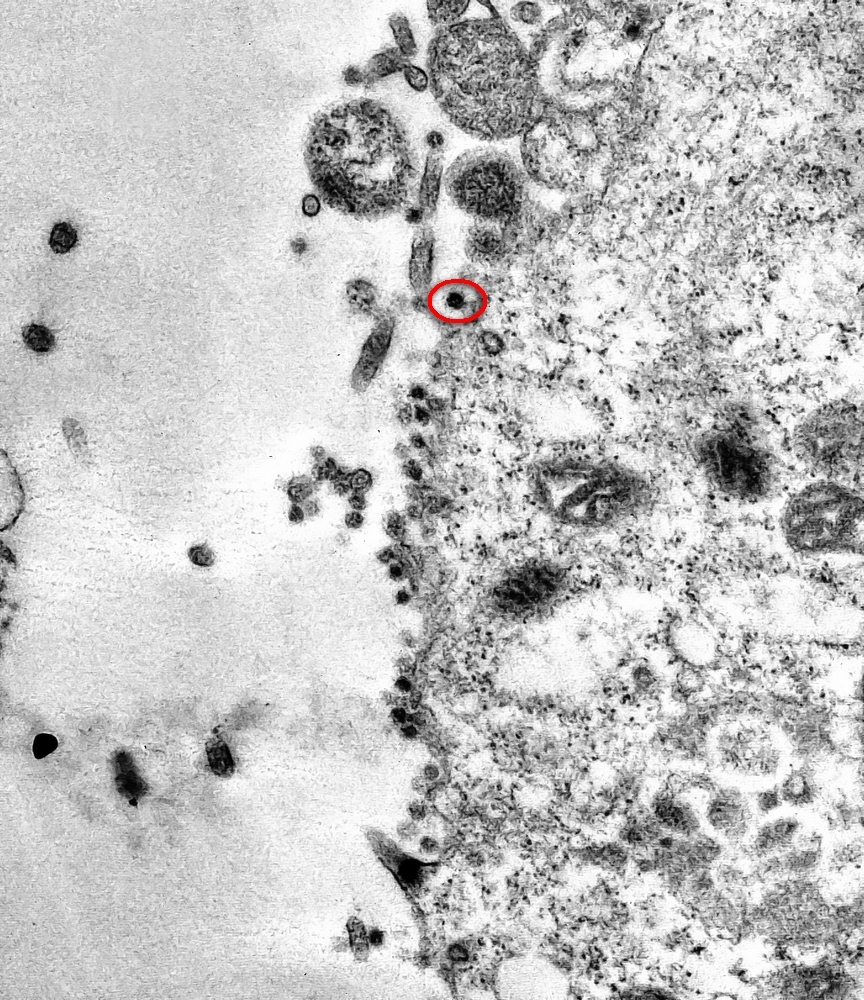 Using its “crown”, the virus (the small black dots in the image) binds to the cell membrane.Source: IOC / Fiocruz / Disclosure
Using its “crown”, the virus (the small black dots in the image) binds to the cell membrane.Source: IOC / Fiocruz / Disclosure
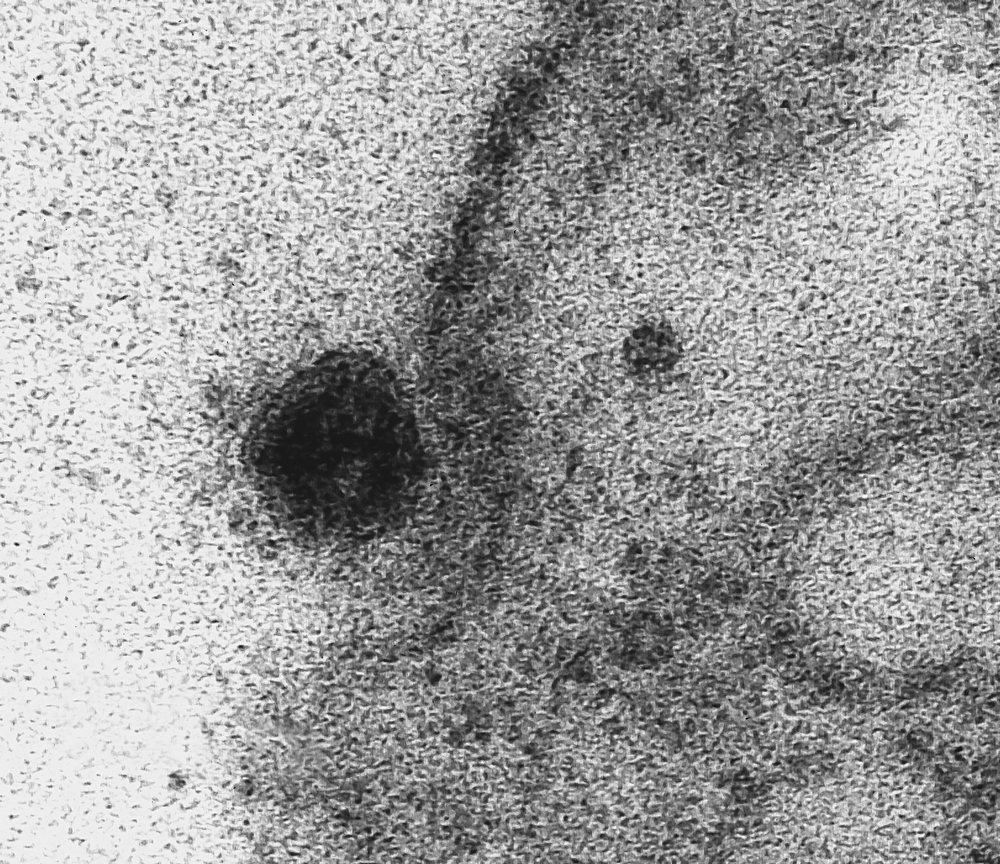 By tricking the enzyme receptor, the virus gets “permission” to enter the cell.Source: IOC / Fiocruz / Disclosure
By tricking the enzyme receptor, the virus gets “permission” to enter the cell.Source: IOC / Fiocruz / Disclosure
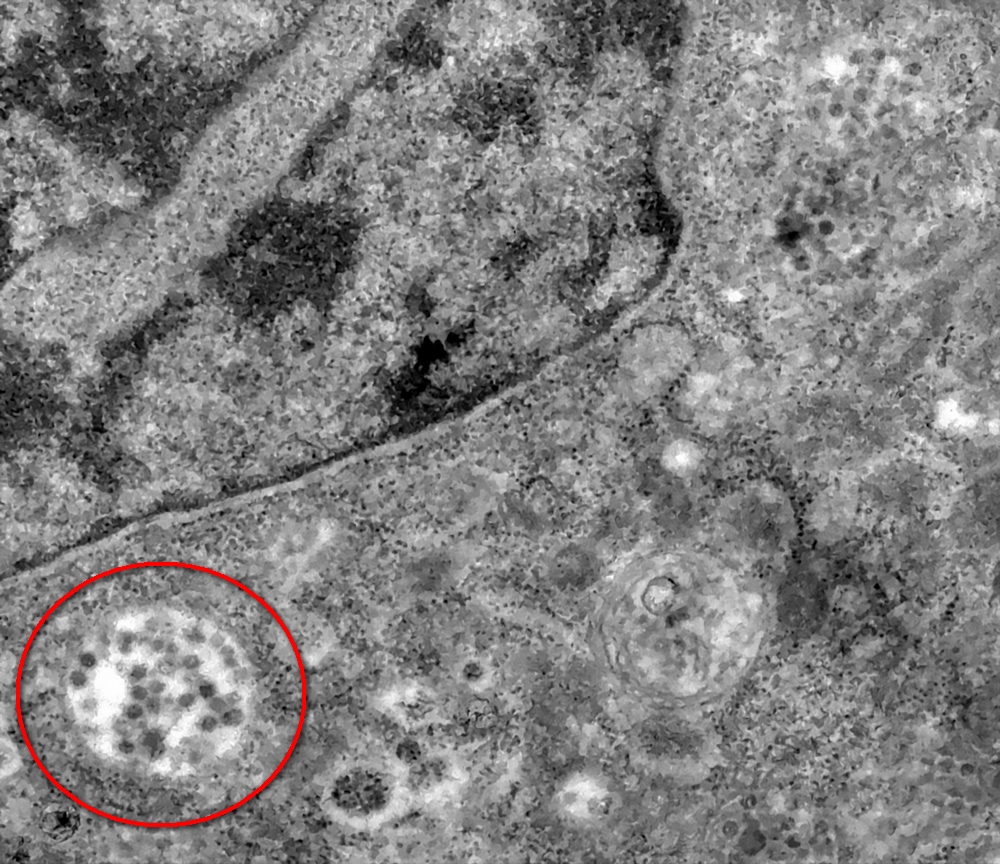 The virus uses everything it finds to produce copies of itself (in the image, the cell, replete with replicas of SARS-CoV-2).Source: IOC / Fiocruz / Disclosure
The virus uses everything it finds to produce copies of itself (in the image, the cell, replete with replicas of SARS-CoV-2).Source: IOC / Fiocruz / Disclosure
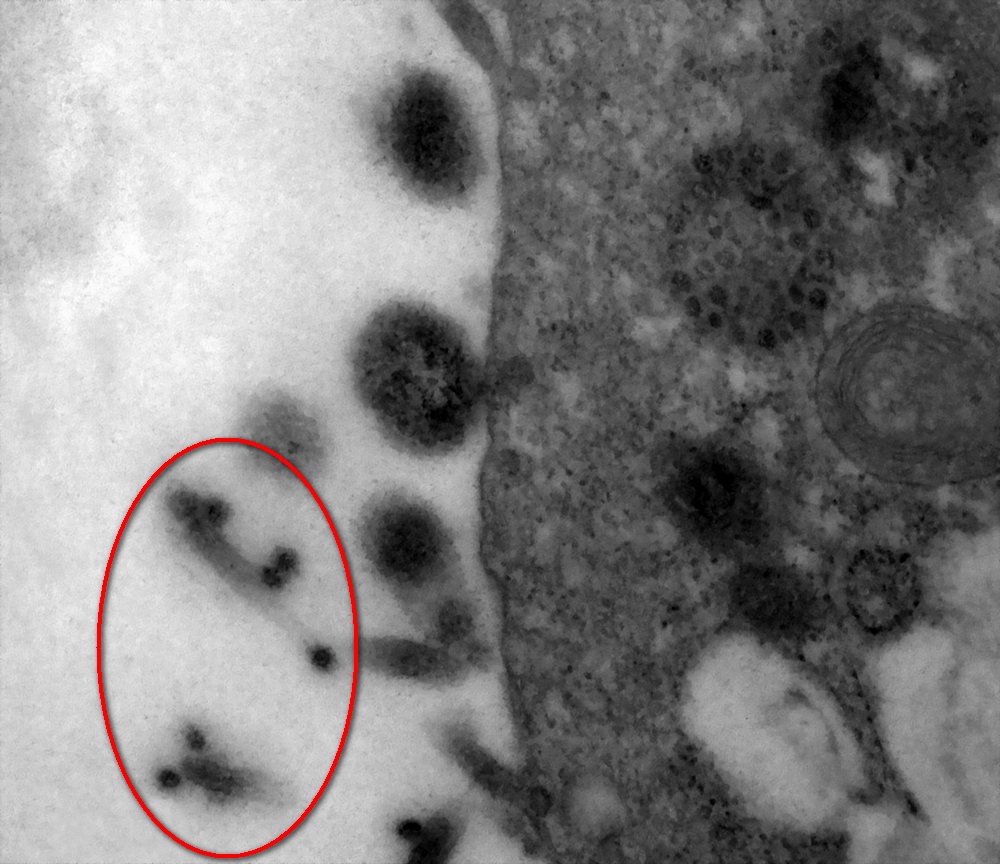 Eventually, the infected cell breaks down and thousands of copies of SARS-CoV-2, which still carry pieces of the membrane, continue to restart the cycle.Source: IOC / Fiocruz / Disclosure
Eventually, the infected cell breaks down and thousands of copies of SARS-CoV-2, which still carry pieces of the membrane, continue to restart the cycle.Source: IOC / Fiocruz / Disclosure
This receptor can be found on the surface of the cells that make up the alveoli, which is why the virus is so dangerous: it reproduces both in the nose and throat and in the lungs.
That’s exactly why scientists at the Berlin Institute of Health and the Thorax Clinic at Heidelberg University Hospital focused on discovering which cells in the respiratory system are primary targets for SARS-CoV-2, using a study that sought to determine why people never smokers develop lung cancer.
According to them, the covid-12 virus selects progenitor cells (similar to stem cells), the main responsible for the production of SARS-CoV-2 receptors. “Knowing which cells are attacked, we can develop targeted therapies,” he explained to BBC Investigator Michael Kreuter.
The most promising vaccine on the way
Using previous studies and cutting the way in the search for a vaccine was what researchers at the University of Pittsburgh School of Medicine did. USA, to create PittCoVacc (an acronym for Pittsburgh Coronavirus Vaccine) Uses, as in current flu vaccines, pieces of viral protein to trigger the immune reaction.
PittCoVacc causes the production of specific antibodies against SARS-CoV-2 in sufficient quantity to neutralize the virus. “After SARS-CoV in 2003 and MERS-CoV in 2014, we knew exactly how to fight this new virus. So it is important to fund vaccine research. You never know when the next pandemic will come,” said microbiologist Andrea Gambotto of the Pitt School of Medicine.
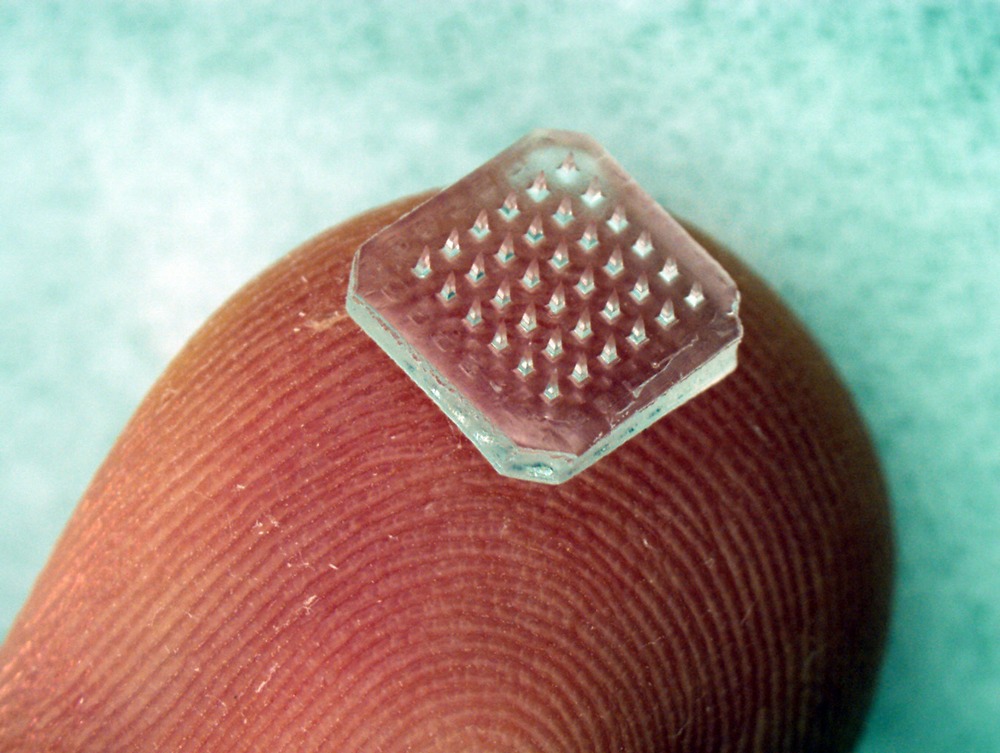 The new vaccine, if approved, will be applied through a microneedle patch.Source: Georgia Tech Research / Disclosure
The new vaccine, if approved, will be applied through a microneedle patch.Source: Georgia Tech Research / Disclosure
The vaccine is administered through a patch the size of a finger tip. Called a “microneedle array,” it looks like a small dressing, containing 400 tiny needles made from sugar and fragments of the virus’s protein. When applied to the skin, they are completely absorbed by the body.
Also read: