An article published Friday in the New England Journal of Medicine suggests that a low-cost steroid may be a valuable treatment for severe COVID-19, based on encouraging preliminary findings from last month.
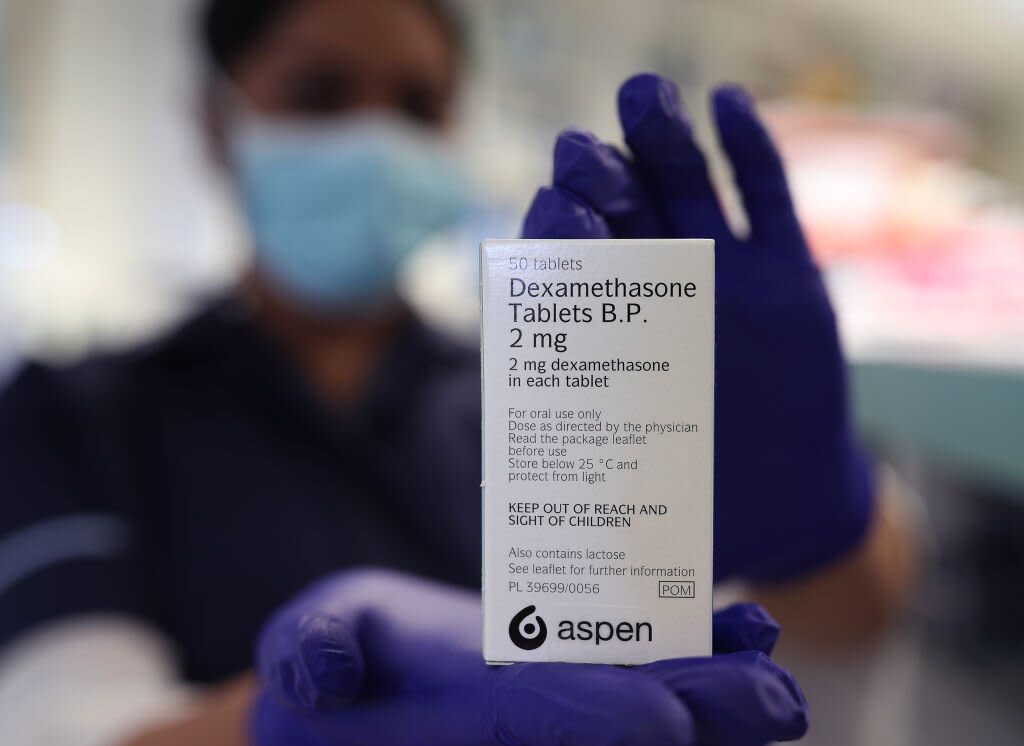
In June, UK researchers reported that dexamethasone, a cheap and widely available steroid that can reduce inflammation in the body, appeared to reduce the risk of death by one-third among patients with severe COVID-19. Professionals in the UK started using dexamethasone the same day the results were announced, but some medical experts were more cautious, arguing that conclusions should not be drawn without seeing the full results of the trial.
Those results were published today in NEJM, and seem to support what was announced last month. Dexamethasone had a measurable benefit for COVID-19 patients sick enough to require respiratory support, but had no such benefit, and even showed the potential for some possible harm, for patients with milder disease.
Approximately 2,100 people hospitalized for confirmed or suspected COVID-19 were randomly assigned to receive a 10-day course of dexamethasone in addition to standard COVID-19 care, while approximately 4,300 received standard care alone. About 16% of patients (in general, both those who received dexamethasone and those who did not) received mechanical ventilation, 60% received only oxygen, and 24% did not receive respiratory support.
After 28 days, 482 patients taking dexamethasone had died, compared to approximately 1,110 of the patients who were not taking it. That means that approximately 23% of the dexamethasone patients died, compared to approximately 26% of the other patients.
It may not seem like a terribly significant difference, but the researchers found a considerable benefit for the sickest patients in the sample: those who require mechanical ventilation to survive. About 30% of these patients died with dexamethasone, compared to 41% of those who did not take it. A minor but still significant benefit was also seen for patients receiving oxygen without invasive ventilation.
Meanwhile, dexamethasone did not provide any benefit for patients who did not need respiratory support. In fact, among patients with these milder cases, those who took dexamethasone were more likely to die, approximately 18% of them did, compared to 14% of those who received standard care alone.
Logically, the anti-inflammatory drug seemed to work better in patients with greater inflammation. Patients who had been symptomatic for at least a week, and therefore likely had developed some inflammatory lung damage, appeared to perform better on the steroid than patients with newer symptoms, who may not have experienced much inflammation.
“The beneficial effect of glucocorticoids is likely [like dexamethasone] in severe viral respiratory infections it depends on selecting the right dose, at the right time, in the right patient, ”the researchers write in the document. “High doses can be more harmful than helpful, as can such treatment given at a time when viral replication is paramount and inflammation is minimal.”
While publication of the document is an encouraging step, the preliminary research has yet to be validated and replicated by other researchers. The researchers also note that because they were aiming to publish the results as soon as possible to meet the demand for new therapies, they did not collect some data on secondary and long-term outcomes.