[ad_1]
Upon arrival at the National Cancer Institute (IMI), we are immediately referred to a polyclinic where a blood test will be performed. It shows if a person has a history of COVID-19 and if they are immune to this infection.
According to Professor Sonata Jarmalaitė, director of IMI, the tests are of various kinds, and the tests at this institution were started due to the fact that cancer patients are in a particularly high risk group, therefore it is necessary ensure your safety.
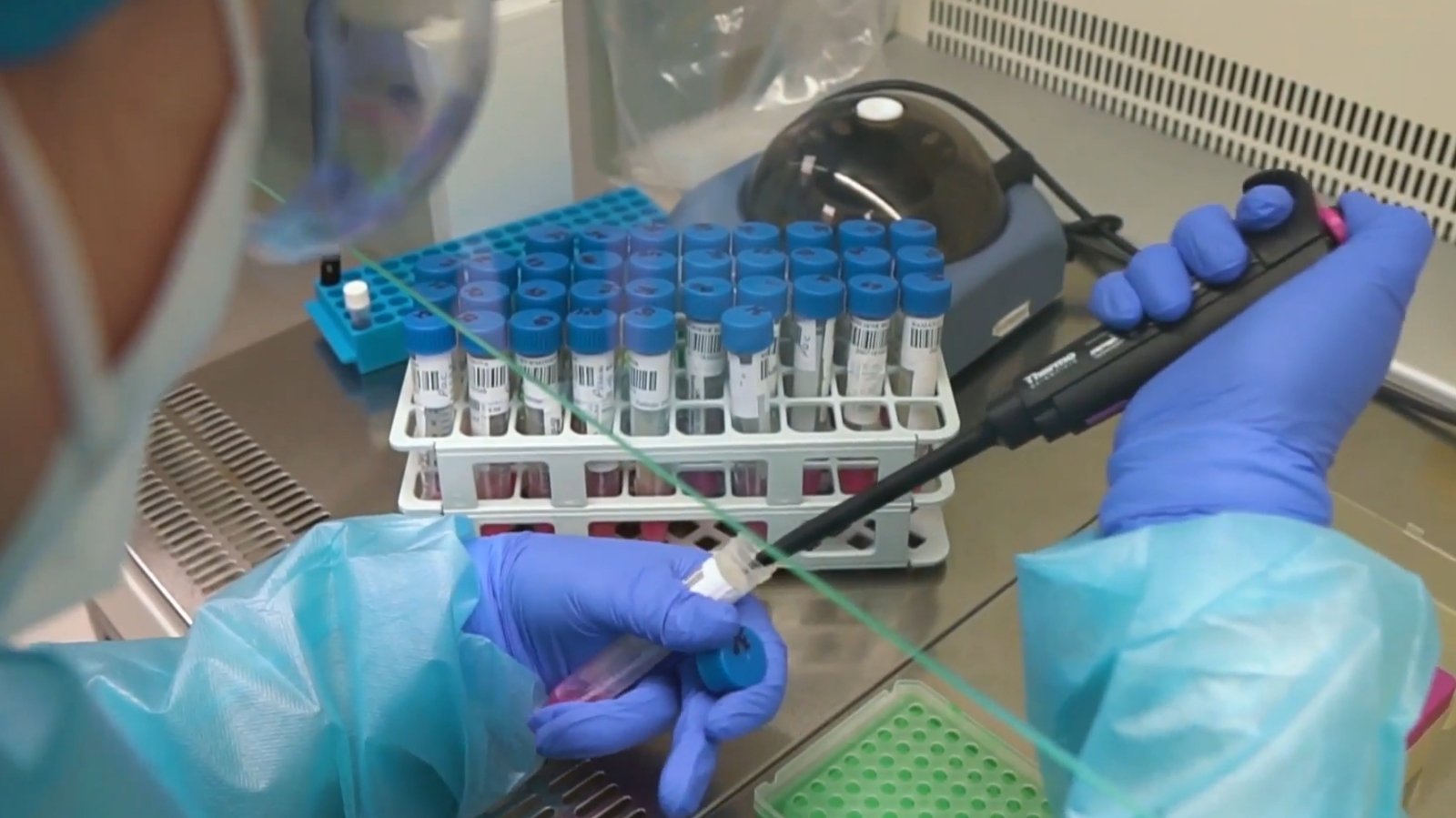
One of the COVID-19 tests is a blood sample.
“If we want to know if we have ever been in contact with a virus and if an immune response has developed, we are testing the blood and we are already testing the result of a human immune response in the blood that has developed antibodies specifically against this virus” . These blood tests are done in several ways, “said the professor.
Once the blood test has been performed, the patient is sent to pick up a special label, which is an identification number that is attached to the tubes. The tube with the patient’s blood continues to travel to the laboratory.

“The blood is delivered to the laboratory: a nurse or an assistant brings it from the procedure room, they put us on the support and then the blood travels to the centrifuge, where it takes 15 minutes. The serum is separated from the red blood cells and the The test is done from the serum, ”said doctor Birutė Nekrošienė from Biutė.
Interestingly, not only COVID-19 antibody tests but also cancer markers are performed with the same device.
“We are starting the machine and there should be a response in 25 minutes. <...> The green light means that the process has already started and now in about 20 minutes, half an hour there will be a response, the light will come on and then we will know if the test is positive or negative, “said B. Nekrošienė.
After a while, the result of the blood test becomes clear.

“Your serological test is negative – 0.065. The limit of the test is one, if it is more than one, it means that you have antibodies against COVID-19. This means that you are not sick and you do not have immunity to this virus” – The journalist from Delfi Tito Atraškevičius presented the results of the blood test to the main coordinator dr. Rasa Sabaliauskaitė.
The next stop is a nasopharyngeal exam.
We are traveling to another stop, where another examination is awaiting, this time smears of the nasopharynx and throat will be taken. Such a study shows whether the patient is currently infected with coronavirus.

“If we want to know if a patient has an infection and if the disease can start, we do a genetic test. The genetic test is informative almost immediately after the infection enters the nasopharynx,” said Professor S. Jarmalaitė.
Initially, preparations are made, a sticker is attached, sterile smear tubes are taken, and a sample is taken from the mouth. The second sample is from the nasopharynx.
A napkin, tube, and these samples are taken to a genetic laboratory where biological manipulations will be performed for approximately 5-6 hours.
Ordinary people will not enter this part of the building: the laboratory is working with a virus, making it extremely dangerous.
Cleanliness and sterility are paramount. To access the IMI clean room, it is necessary to disinfect your hands several times well and wear a special protective suit, as biological reactions will occur in this area.
“You should first put on a bathrobe. They are designed to protect us from virus splashes, either from samples or from our own crystal cells. Every time we change, we always disinfect our hands,” said biologist Ieva Vaicekauskaitė.
Agnė Šeštokaitė, a junior researcher, talks about how the examination of a smear from the nasopharynx continues.

“We analyze the samples received today, as well as register them in the system and finally incubate them, for security reasons. After half an hour at a temperature of 56 degrees, the virus becomes less active, so it is not possible to become infected as easily, says A. Šeštokaitė.
– We also use another reagent: lysis. First we will dispense the lysis reagent, we will finally dispense the samples, and then our plate with all the samples will travel through this corridor to the person pouring the PCR reagents. “
Several other stages of the study.
We go to another laboratory where we work with patient samples. Several layers of protective gear and a whispering device emit a lot of heat, so in the lab it is very hot, the girls even joke that we are in the sauna.
After pipetting in the laboratory, wait for the next step: the apparatus will perform a reaction, after which it will be clear whether the subjects are infected with the corana virus or not.

Coronavirus study
© Stop frame
The samples are then returned to the centrifuge, which is spun for approximately one minute.
“The next step is to see if there are bubbles, because when we put them in another device there should be no bubbles.” When you put it on the board, a special program will run on the computer recommended by the reagent manufacturer. After an hour and a half, because this study takes so long, we see the results on the computer. The last stop is the analysis of the results, but from a practical point of view, bottling is the last stop, “said Justina Gaiževska, medical genetics and junior researcher.
Therefore, the practical part of the study has already been completed; now the analysis of the results remains in a computer program, which will show if there are infected cases.

Coronavirus study
© Stop frame
“Not only samples are placed, but also controls on the plate, a negative control that shows contamination and without curves, without banquets. And a positive control that contains the virus and from which we can evaluate if the patient is sick. If there are no curves red means the test is negative. If there were red curves it would be a sign to us that this patient is infected with the virus, “said J. Gaiževska.
The results obtained will soon be entered into the electronic system “esveikata.lt”, where both doctors and patients can see the final result of the study, that is, to find out if a person is infected with the COVID-19 virus or not.
It is strictly prohibited to use the information published by DELFI on other websites, in the media or elsewhere, or to distribute our material in any way without consent, and if consent has been obtained, DELFI must be cited as the source.
[ad_2]