
[ad_1]
– What are COVID-19 vaccines and how do they work?
– COVID-19 vaccines are drugs that help the human body to develop an immune response against the new SARS-CoV-2 virus and thus protect against the COVID-19 disease it causes.
Different types of vaccines work differently, but the principle of all jobs is to trigger an immune response by helping the body produce memory immune cells – T, B lymphocytes, and protective antibodies. Generally, several weeks must elapse after vaccination to produce enough memory cells, antibodies, and protection against COVID-19 infection. If a person is subsequently infected with the SARS-CoV-2 virus, their immune system will be able to recognize and fight the virus to prevent COVID-19 infection.
Like all medicines, the quality, safety and efficacy of vaccines are studied in laboratories after development, followed by clinical trials in several stages. Only after successfully completing all stages of vaccine development are vaccines developed in daylight.

Vaccination against coronavirus in the Kaunas clinics
© Kaunas Clinics
– How are COVID-19 vaccines distributed?
– The mechanism of action currently identifies three main types of COVID-19 vaccines that are in the final stages of clinical trials or already registered with the European Medicines Agency (EMA) and used for human vaccination.
MRNA vaccines. The mRNA vaccines contain genetic information from the virus that allows human cells to produce only the needle surface protein specific for SARS-CoV-2. Once produced, the vaccine substance is destroyed in the human body and the immune system, after recognizing the foreign protein, it begins to produce antibodies and activates the T cells. After vaccination, when the SARS-CoV virus -2 enters the human body, the immune system recognizes its surface protein, activates the immune response, and destroys the virus. Currently, two EVA registered and approved mRNA vaccines are used for vaccination: Pfizer-BioNTech Comirnaty and Moderna TX Moderna. Although mRNA vaccines are new, scientists have known the principle of their action for decades. In the past, they have been working to find effective protection against influenza, Zika, rabies, and CMV viruses.
Vector vaccines. These vaccines are made using a harmless, attenuated virus other than SARS-CoV-2, such as adenovirus. The genetic information from the SARS-CoV-2 virus has been incorporated into this COVID-19 disease-free virus. When this vector virus (vector) is injected into the human body with the vaccine, information is obtained on how to produce the surface protein of the SARS-CoV-2 virus. It is recognized by the immune system and responds accordingly by activating the production of antibodies against the T and B lymphocytes in which the information is stored. After being vaccinated with SARS-CoV-2, the immune system is activated and the virus dies, thus preventing COVID-19. Vector vaccines include AstraZeneca, which has successfully completed all stages of vaccine development and is currently being evaluated by EVA for registration and availability of COVID-19 vaccines.
Protein subunit vaccines. These vaccines contain a harmless protein from the SARS-CoV-2 virus. After vaccination, the human body’s immune system recognizes a foreign protein that does not belong to the body and activates immune T cells and antibodies, and defensive information is stored in memory cells. Later, when infected, memory cells recognize the virus, activating the immune system, which destroys the virus and protects it against COVID-19 disease.
– How is COVID-19 mRNA vaccinated?
– Both currently licensed mRNA vaccines are administered intramuscularly in the upper arm at 0.3 ml (Pfizer-BioNTech Comirnaty) or 0.5 ml (Moderna). The vaccine is administered in two doses, 21 or 28 days apart, depending on the vaccine being administered. Both doses must be administered with the same vaccine.
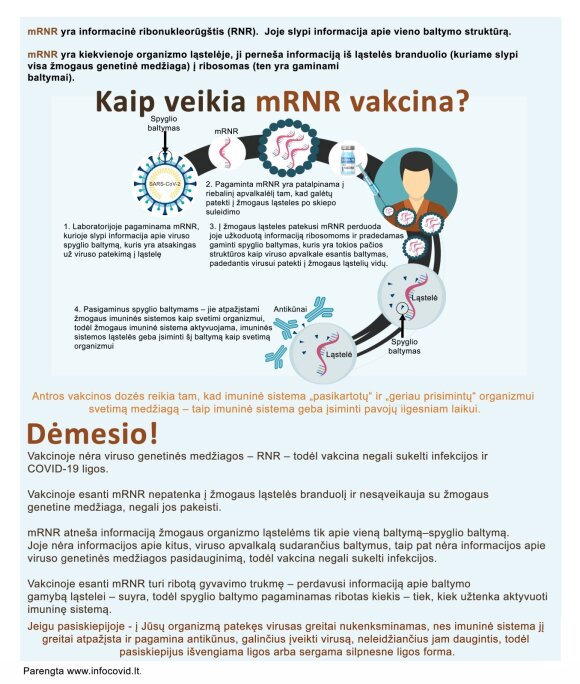
How does the mRNA vaccine work?
© Kaunas Clinics
– What is the effectiveness of mRNA vaccines?
– The efficacy of mRNA vaccines in clinical trials was 94.1 to 95% among subjects vaccinated with the two doses.
The efficacy of Pfizer-BioNTech Comirnaty did not differ between subjects with chronic lung disease, diabetes, arterial hypertension, asthma and those with a body mass index ≥ 30 kg / m2 and was 95%.
The effectiveness of the Moderna vaccine in a clinical trial in patients with chronic lung, heart, liver, diabetes or HIV disease was 91%.
– When and how long does immunity to SARS-CoV-2 develop after vaccination with mRNA?
– Immunity to the SARS-CoV-2 virus after vaccination with the mRNA vaccine develops at least 14 days after the second dose, but the duration is unknown. Vaccinated individuals will be followed in clinical trials for another two years to gain more scientific insight into the duration of the immune response.
– Who can be vaccinated with the COVID-19 mRNA vaccines?
– Pfizer-BioNTech Comirnaty can be given to people over 16 years of age. The Moderna vaccine can be given to people over 18 years of age.
– Who cannot be vaccinated with COVID-19 mRNA vaccines?
– These vaccines should not be given to people who have ever had an allergic or anaphylactic-allergic reaction to any of the ingredients in the vaccine.

Vaccination against coronavirus in the Kaunas clinics
© Kaunas Clinics
– What are the side effects of mRNA vaccines?
– Adverse events seen in clinical trials with mRNA vaccines were not different from other vaccines, occurred more frequently after the second dose, and were more common in patients younger than 55 years. in a group of people.
The most common side effects after the second dose of the vaccine were mild to moderate: local reaction at the injection site (pain, redness, swelling), tiredness, headache, muscle and joint pain, chills, fever.
Of the 18,801 subjects who received at least one dose of the vaccine in the Pfizer-BioNTech Comirnaty clinical trial, four had facial nerve palsy.
Among the 15,184 subjects who received at least one dose of the vaccine in Moderna’s clinical trial, facial nerve palsy occurred in three. These cases of facial nerve palsy were no more common than in the general population, so there is currently no clear reason to believe they were caused by vaccination.
Prepared by www.infocovid.lt
It is strictly prohibited to use the information published by DELFI on other websites, in the media or elsewhere, or to distribute our material in any way without consent, and if consent has been obtained, it is necessary to indicate DELFI as the source .
[ad_2]