[ad_1]
In 2018 psychiatrist Oleguer Plana-Ripoll was wrestling with a puzzling fact about mental disorders. Did you know that many people have multiple conditions: anxiety and depression, for example, schizophrenia and bipolar disorder. He wanted to know how common it was to have more than one diagnosis, so he had in his hands a database containing the medical details of around 5.9 million Danish citizens.
He was surprised by what he found. Each mental disorder predisposes the patient to any other mental disorder, no matter how different the symptoms are.one. “We knew that comorbidity was important, but we did not expect to find partnerships for all couples,” says Plana-Ripoll, who resides at Aarhus University in Denmark.
The study addresses a fundamental question that has bothered researchers for more than a century. What are the roots of mental illness?
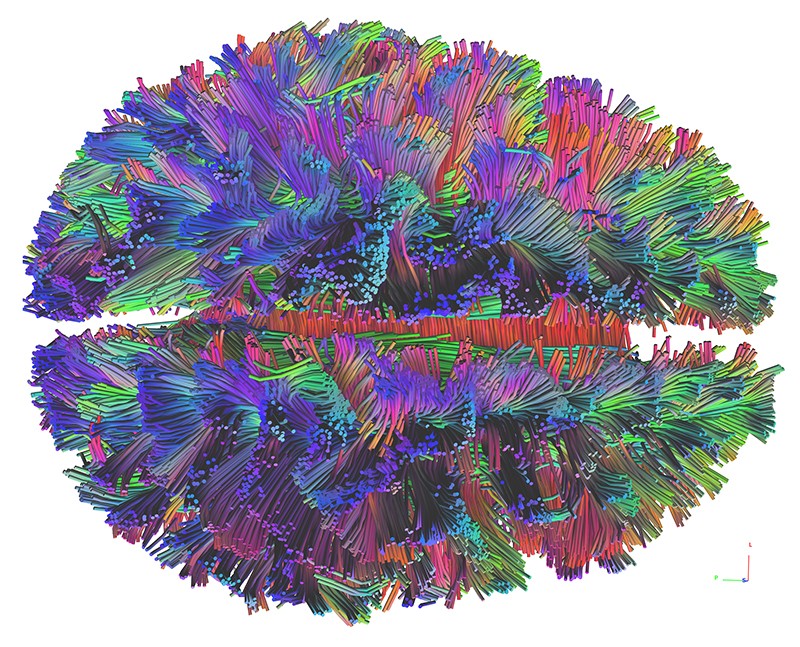
Hoping to find an answer, scientists have amassed a tremendous amount of data over the past decade, through studies of genes, brain activity, and neuroanatomy. They have found evidence that many of the same genes underlie apparently different disorders, such as schizophrenia and autism, and that changes in the brain’s decision-making systems could be involved in many conditions.
Researchers are also dramatically rethinking theories of how our brains fail. The idea that mental illness can be classified into distinct and discrete categories such as “anxiety” or “psychosis” has been largely refuted. Instead, the disorders shade each other and there are no hard dividing lines, as the Plana-Ripoll study clearly demonstrated.
Now, researchers are trying to understand the biology that underlies this spectrum of psychopathology.
They have some theories. Perhaps there are several dimensions of mental illness, so depending on how a person scores in each dimension, they may be more prone to some disorders than others. An alternative and more radical idea is that there is a single factor that makes people prone to mental illness in general: the disorder they develop is then determined by other factors. Both ideas are taken seriously, although the multi-dimensional concept is more widely accepted by researchers.
The details are still unclear, but most psychiatrists agree that one thing is clear: The old system of categorizing mental disorders in neat boxes does not work. They also hope that eventually replacing this framework with a biology-based one will lead to new drugs and treatments. The researchers aim to reveal, for example, the key genes, brain regions, and neurological processes involved in psychopathology, and target them with therapies. Although it might take a while to get there, says Steven Hyman of the Broad Institute of MIT and Harvard in Cambridge, Massachusetts, “I’m optimistic in the long run if the field really does its job.”
A heterogeneous mix of disorders
The most immediate challenge is figuring out how to diagnose people. Since the 1950s, psychiatrists have used a comprehensive volume called Diagnostic and Statistical Manual of Mental Disorders, currently in its fifth edition. Lists all recognized disorders, from autism and obsessive compulsive disorder to depression, anxiety, and schizophrenia. Each is defined by symptoms. The inherent assumption is that each disorder is different and arises for different reasons.
However, even before the DSM-5 It was published in 2013, many researchers argued that this approach was flawed. “Any clinician could have told him that the patients had not read the DSM and it didn’t fit the DSM“Says Hyman, who helped write the fifth edition of the manual.
Few patients fit each ordered set of criteria. Instead, people often have a mix of symptoms of different disorders. Even if someone has a fairly clear diagnosis of depression, they often have symptoms of another disorder like anxiety. “If you have one disorder, you are much more likely to have another,” says Ted Satterthwaite, a neuropsychiatrist at the University of Pennsylvania in Philadelphia.
This implies that the way doctors have divided mental disorders is incorrect. Psychiatrists have tried to solve this by dividing the disorders into increasingly finer subtypes. “If you look at the way that DSM it has evolved over time, the book gets thicker and thicker, “says Satterthwaite. But the problem persists: the subtypes remain a poor reflection of the symptom groups that many patients have.
As a result, the world’s leading funder of mental health science, the US National Institute of Mental Health. UU., It changed the way in which it financed the investigation. Starting in 2011, it began to demand more studies on the biological basis of disorders, rather than their symptoms, in a program called Research Domain Criteria. Since then there has been an explosion of research on the biological foundations of psychopathology, with studies focused on genetics and neuroanatomy, among other fields. But if the researchers hoped to demystify psychopathology, they still have a long way to go: The key finding has been how complex psychopathology really is.
Controversial groups
Clinically, evidence that symptoms cross disorders, or that people often have more than one disorder, has only been strengthened. For this reason, although individual symptoms, such as mood disturbances or deficiencies in reasoning, can be reliably diagnosed, it is difficult to assign patients a general diagnosis as “bipolar disorder”.
Even seemingly separate disorders are linked. In 2008, geneticist Angelica Ronald, then at King’s College London Institute of Psychiatry, and her colleagues discovered that autism and attention deficit hyperactivity disorder (ADHD) overlapped. “At the time, you weren’t allowed to be diagnosed with both conditions,” says Ronald; this was due to a rule in an earlier version of the DSM. But she and her team found that autism and ADHD traits were strongly correlated and partially under genetic control.2.
Furthermore, there appear to be groups of symptoms that cross the boundaries of the disorders. A 2018 study3 examined people who had been diagnosed with major depression, panic disorder, or post-traumatic stress disorder (PTSD). The volunteers were evaluated based on their symptoms, cognitive performance and brain activity. The researchers found that the participants were divided into six groups, characterized by different mood states, such as “tension” and “melancholy.” Groups traverse all three diagnostic categories as if they were not there.
Many now agree that the diagnostic categories are incorrect. The question is, with biology as a guide, what should psychiatric diagnosis and treatment be like?
Multiple dimensions
An outstanding model is that there are a series of neuropsychological features or “dimensions” that vary from person to person. Each trait determines our susceptibility to certain types of disorder. For example, someone may be prone to mood disorders like anxiety, but not to thought disorders like schizophrenia.
This is similar to the way psychologists think about personality. In one model, five personality traits, such as consciousness and neuroticism, describe most of the variation in human personalities.
Some psychiatrists are already trying to reimagine their discipline with dimensions in mind. In the early 2010s, there was a push to remove the categories of disorders of the DSM-5 in favor of a “dimensional” approach based on individual symptoms. However, this attempt failed, in part because funding for medical care and patient care have accumulated around DSMHowever, other disorder catalogs have shifted toward dimensionality. In 2019, the World Health Assembly approved the latest International Classification of Diseases (called ICD-11), in which some psychopathologies were recently broken down using dimensional symptoms rather than categories.
The challenge to the dimensionality hypothesis is obvious: how many dimensions are there and what are they? Satterthwaite calls this “a very big problem”.
A popular theory4 4, backed by many studies over the past decade, defends only two dimensions. The first includes all “internalization” disorders, such as depression, in which the primary symptoms affect a person’s internal state. This is in contrast to “externalization” disorders, such as hyperactivity and antisocial behavior, in which a person’s response to the world is affected. If someone has been diagnosed with two or more disorders, studies suggest they are likely to be in the same category.
But studies combining large amounts of brain imaging data with machine learning have yielded different numbers, even in studies by the same laboratory. Last year Satterthwaite and his group published a study.5 5 of 1,141 young people who had internalization symptoms and found that they could be divided into two groups based on their brain structure and function. In 2018 Satterthwaite led a similar study.6 6 and identified four dimensions, each associated with a different pattern of brain connectivity.
In short, a future version of DSM It could have chapters dedicated to each dimension, says Hyman. These could list the disorders that are clustered within each, as well as their symptoms and any biomarkers derived from the underlying physiology and genetics. Two people who had similar symptoms but different sets of neuroanatomical mutations or alterations could be diagnosed and treated differently.
In the genes
A pillar of this future approach is a better understanding of the genetics of mental illness. In the past decade, studies of psychopathological genetics have become large enough to draw solid conclusions.
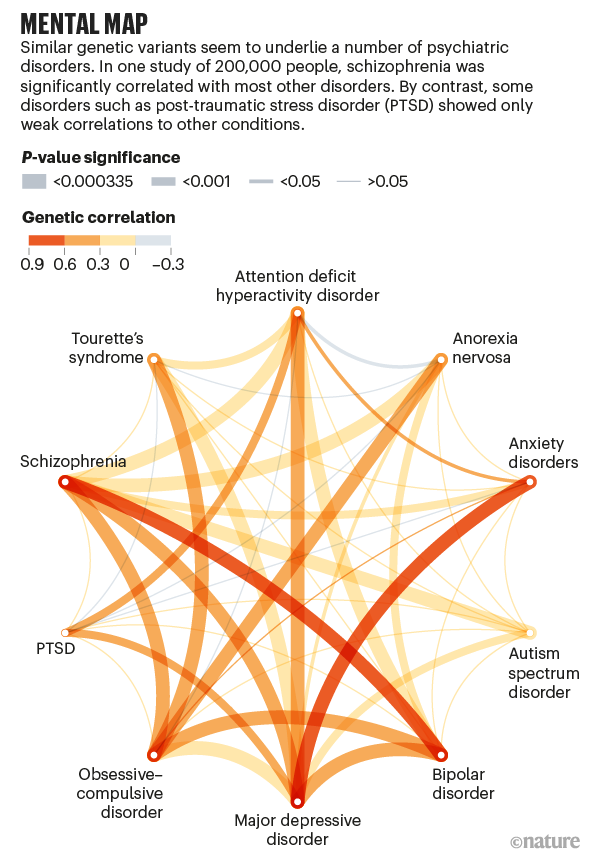
Studies reveal that no single gene contributes much to the risk of psychopathology; instead, hundreds of genes each have a small effect. A 2009 study7 7 He discovered that thousands of genetic variants were risk factors for schizophrenia. Many were also associated with bipolar disorder, suggesting that some genes contribute to both disorders.
This does not mean that the same genes are involved in all brain disorders: far from it. A team led by geneticist Benjamin Neale at Massachusetts General Hospital in Boston and psychiatrist Aiden Corvin at Trinity College Dublin discovered in 2018 that neurological disorders such as epilepsy and multiple sclerosis are genetically distinct from psychiatric disorders such as schizophrenia and depression.8 (see “Mind Map”).
All of these studies looked at common variants, which are the easiest to detect. Some recent studies instead focused on extremely rare variants, which suggest genetic differences between the disorders. A study of more than 12,000 people.9 9 They found that people with schizophrenia had an unusually high rate of ultra-rare mutations, and that they were often unique to an individual.
The result is a disaster. It is difficult to predict what risk factors the conditions go through. “Some of them are widely shared in psychopathology,” says Neale, “while others are slightly more specific to one or more forms of psychopathology.”
the P factor
Some psychiatrists have put forward a radical hypothesis that they hope will allow them to make sense of the chaos. If the disorders share symptoms or coexist, and if many genes are involved in multiple disorders, then perhaps there is a single factor that predisposes people to psychopathology.
The idea was first proposed in 2012 by public health specialist Benjamin Lahey of the University of Chicago at Illinois.10. Lahey and colleagues studied symptoms in 11 disorders. They used statistics to examine whether the pattern could best be explained by three different dimensions, or by those three together with a “general” bias. The model worked best if the general factor was included.
The following year, the hypothesis received more support, and a striking name, from husband and wife psychologists Avshalom Caspi and Terrie Moffitt at Duke University in Durham, North Carolina. They used data from a long-term study of 1,037 people and found that most of the variation in symptoms could be explained by a single factor.eleven. Caspi and Moffitt called this the ‘P factor’. Since 2013, multiple studies have replicated their main finding.
Caspi and Moffitt were clear that the P The factor couldn’t explain everything, and it didn’t speculate on its underlying biology, speculating only that a set of genes could mediate it. Others have proposed that the P The factor is a general predisposition to psychopathology, but that other factors (stressful experiences or other genetic alterations) push a person towards different symptoms12. But if it’s real, it has a surprising implication: There could be a single therapeutic target for psychiatric disorders.
There are already indications that widespread treatments may work as well as targeted therapies. A 2017 study13 randomized individuals with anxiety disorders, such as panic disorder or obsessive compulsive disorder, to receive therapy for their specific disorder or a general approach. Both therapies worked equally well.
Find a physiological basis for P The factor would be the first step towards therapies based on it, but only in recent years have researchers found clues in genetic and neuroanatomical data. A study14 of the genetics of psychopathology in a UK population, for example, identified a genetic ‘ P factor “: a set of genes in which there were variations that contributed to the risk of psychopathology.
Meanwhile, other groups have looked for a neuroanatomical change that occurs in multiple psychopathologies. The results are intriguing, but contradictory.
A studyfifteen from six psychopathologies found that the gray matter of the brain contracted in three regions involved in the processing of emotions: the dorsal anterior cingulate, the right insula and the left insula. But subsequent studies by Adrienne Romer, a clinical psychologist now at Harvard Medical School and McLean Hospital in Belmont, Massachusetts, identified a totally different trio of regions with roles that include managing basic body functions and movement.sixteen – the protuberance, the cerebellum and part of the cortex. One key to making sense of this might be to focus on the executive function of the brain: the ability to regulate behavior by planning, paying attention, and resisting temptation, which is based on many regions of the brain. Romer and Satterthwaite have independently found interruptions in executive function in a variety of psychopathologies.17,18 years – the suspicion is that these interruptions could be the basis of the P factor.
Most scientists agree that what is needed is more data, and many are not convinced by such simple explanations. “I’m a little less certain that this is how it will unfold,” says Neale. At least on the genetic level, he says, there are many disorders, such as PTSD and generalized anxiety disorder, that remain poorly understood.
All of these radical hypotheses are premature, says Hyman. “I think it is a time for much more empirical research rather than great theorizing.”