[ad_1]
Researchers in the United States have identified mutations within severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the agent that causes coronavirus disease 2019 (COVID-19), that can reduce the binding of antibodies to the virus, resulting in that could mediate your escape from immune attack.
The team used a technique called Phage-DMS to profile the escape of this antibody into a surface structure called the spike protein, which the virus uses to bind and infect host cells.
Using blood samples from patients who had recovered from COVID-19, the team tested all possible mutations within the spike protein that could utilize escape pathways within the epitopes that are targeted by convalescent plasma.
The team, from the Fred Hutchinson Cancer Research Center and the University of Washington, found that antibody binding was common in two immunodominant regions, but that there were many unique escape routes within these regions.
These escape mutations also differed between individuals, suggesting that the binding sites of antibodies and escape mutants could vary significantly from person to person.
“We identified a spectrum of individual mutants that were capable of reducing antibody binding and found person-to-person variability in the effect of mutations within immunodominant epitopes,” write Julie Overbaugh and the team.
The findings suggest that people’s responses to a vaccine that targets the spike protein are unlikely to be consistent, the researchers say.
“In the arms race between the humoral immune response and SARS-CoV-2, these results allow us to predict escape routes and predict the emergence of escape mutants,” the team writes.
A pre-printed version of the paper is available from the bioRxiv * server, while the article undergoes peer review.

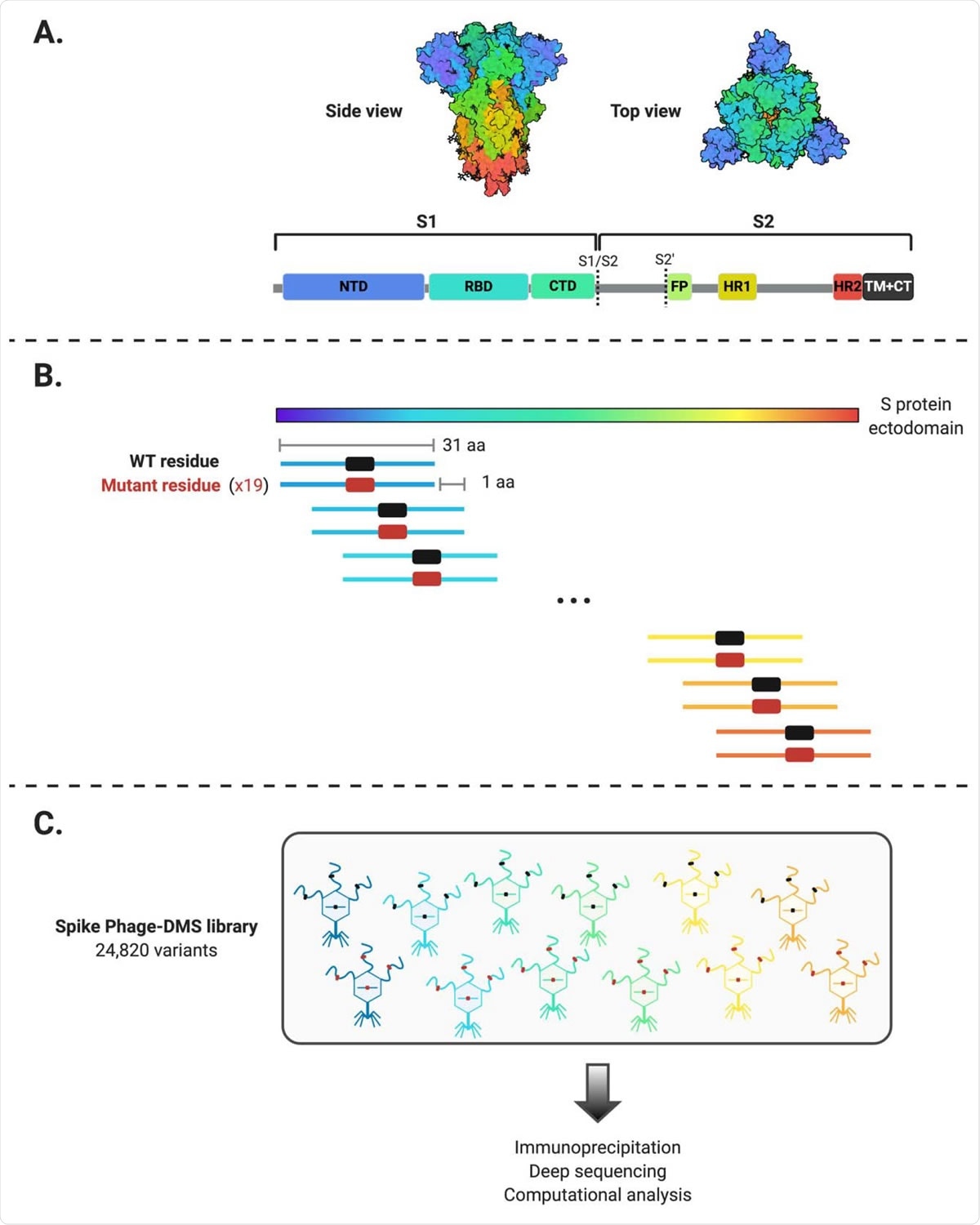
Schematic of the design of the Spike Phage-DMS library. (A) Structure of protein S and location of important protein domains. The structure was created at BioRender.com (PDB: 6VXX) (B) The sequences were computationally designed to encode peptides 31 amino acids in length and to stepwise distribute the ectodomain of the Wuhan-Hu-1 SARS-CoV-2 S protein per 1 amino acid. There are 20 peptides representing the 20 possible amino acids in the central position, containing either the wild-type residue (shown in black) or a mutant residue (shown in red). Within the 31 aa region surrounding the D614G mutation, G614 peptides were also generated in addition to the 20 amino acid variants in the central position. (C) Engineered sequences were cloned into a T7 phage display vector and amplified to create the final Phage-DMS protein S library. This library was then used in deep sequencing and downstream immunoprecipitation experiments with human plasma.
Researchers are not sure if immunity against SARS-CoV-2 is long-lasting
Determining whether immunity to SARS-CoV-2 can be protective in the long term is one of the most pressing challenges facing researchers working to develop vaccines against SARS-CoV-2.
Understanding how the virus might evolve to escape immune protection is critical to answering this question.
The primary viral target of interest to researchers is the spike protein, the structure that initiates host cell attachment and fusion to allow viral entry.
The spike protein is made up of two subunits. Subunit 1 (S1) contains an N-terminal domain (NTD) and a receptor-binding domain (RBD). Subunit 2 (S2) contains a fusion peptide (FP) and two heptad repeat regions (HR1 and HR2), separated by a linker region, that drive fusion of the virus and the host membrane.
Once S1 binds to a host cell through RBD, a proteolytic cleavage occurs within S2 that exposes FP and triggers a series of conformational changes that allow membrane fusion.
Neutralizing antibodies that target RBD have been the main focus of efforts to develop vaccines and antibody therapies. These neutralizing antibodies have been shown to block virus entry in vitro and prevent infection or disease in preclinical models.
“However, studying other coronaviruses has shown that antibodies elicited by infection can target epitope regions outside of the RBD,” say Overbaugh and his colleagues. “Therefore, there may be multiple regions within the SARS-CoV-2 spike protein that can shape the viral immune response. “
Furthermore, given the unusually high transmission rate of SARS-CoV-2 and the high mutability of previous coronaviruses, it is likely that variants will emerge that are capable of evading the immune response.
What did the researchers do?
Previously, Overbaugh and the team developed a method called Phage-DMS to comprehensively map the escape mutations that allowed HIV to prevent the binding of monoclonal antibodies.
The team has now used this technique to identify mutations in the SARS-CoV-2 spike protein that could reduce antibody binding and therefore mediate the escape of antibodies present in the plasma of COVID-19 patients.
What did you find?
The team found that antibody binding was common in two regions: the FP and the HR2 upstream linker region.
The study revealed a spectrum of unique mutants that were capable of reducing antibody binding within these regions.
However, the escape mutations showed variability within these immunodominant regions, as well as person-to-person variability.
What are the implications of the study?
The findings suggest that the evolutionary pattern of the virus is not likely to be driven by a single antibody escape mutation. They also suggest that there will be inter-individual variation in antibody-mediated evolution of the virus.
“Thus, responses to a SARS-CoV-2 spike protein vaccine are likely not uniform, and neither are the escape routes,” the team writes.
The researchers say that FP epitopes and the / HR2 linker region could serve as alternative targets for vaccine and immunotherapy development that could complement efforts focused on RBD.
The team says that S2 in general, especially FP, is highly conserved in coronavirus. These more conserved regions could be important targets for the design of optimal and durable vaccines.
“These studies have defined common and variable escape mutations in COVID-19 patients that will be useful for viral surveillance, particularly as SARS-CoV-2 spike protein-based vaccines are introduced to the population,” they write. the researchers.
Additionally, the Phage-DMS spike protein library used in this study could be used to examine larger cohorts, which could include individuals of different ages and with varying clinical outcomes, Taylor and colleagues suggest.
This could help to “define whether mutations that disrupt antibody binding vary systematically between populations and whether this correlates with clinical outcome or risk of reinfection,” the team concludes.
*Important news
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and therefore should not be considered conclusive, guide clinical practice / health-related behavior, or be treated as established information.