EASK
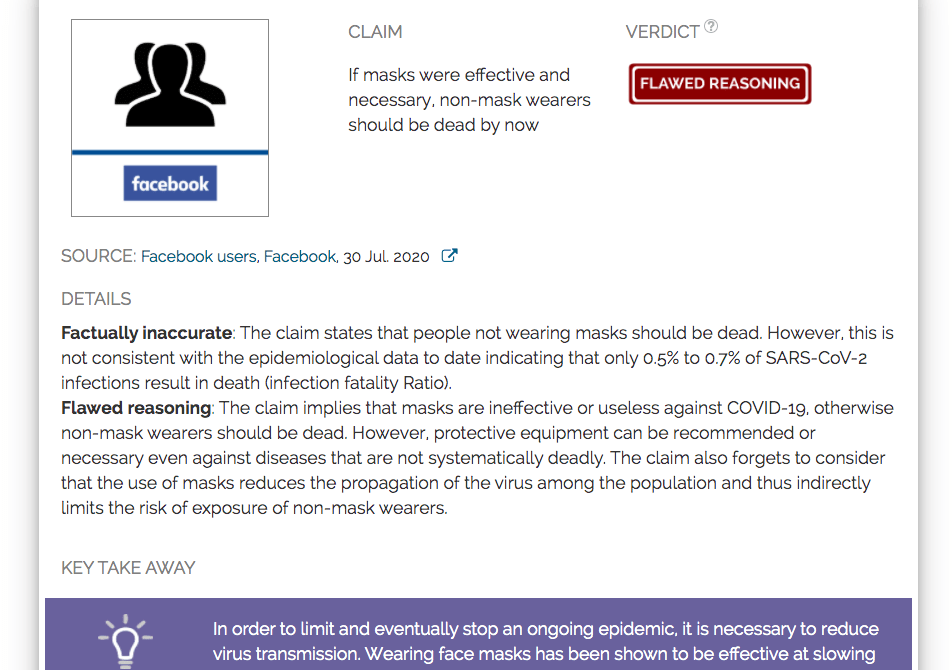
If masks were effective and necessary, non-mask wearers would now have to die

DETAILS
Virtually inaccurate: The recommendation states that people who do not wear masks should be dead. However, this is inconsistent with the epidemiological data to date, which indicate that only 0.5% to 0.7% of SARS-CoV-2 infections lead to death (infection fatal ratio).
Wrong reasoning: The claim implies that masks are ineffective or useless against COVID-19, otherwise non-mask wearers would have to die. However, protective equipment may be recommended if necessary, even against diseases that are not systematically fatal. The claim also forgets to consider that the use of masks reduces the propagation of the virus among the population and thus indirectly limits the risk of exposure of non-mask carriers.
KEY TAKE AWAY

To curb and eventually stop an ongoing epidemic, it is necessary to reduce virus transmission. Wearing face masks has been shown to be effective in slowing the circulation of respiratory viruses such as SARS-CoV-2. Some people who do not wear masks can still stay healthy because exposure to SARS-CoV-2 does not automatically lead to infection or death. In addition, the use of masks by others in the community can also limit the transmission of viruses, thus protecting those who do not wear masks, similar to the immune effect of herd
FULL CLAIM: If masks were effective and necessary, non-mask wearers would now have to die
REVIEW
In August 2020, a post circulating on social media, which received millions of views, questioned how people who did not wear face masks were still alive in the midst of the COVID-19 pandemic. Using the “just ask questions” rhetorical technique, this claim suggests that masks are ineffective as useless against COVID-19. This reasoning is based on the premise that a protective device is only efficient and necessary if 100% of people who do not use it die. Such logic is actually flawed and inconsistent with the available knowledge about the disease.
In fact, it is easy to see that protective equipment can be useful, although not using it will not automatically result in the death of someone. For example, not everyone who gets on a motorcycle without a helmet dies, even though such protection is effective and highly recommended.
Second, not everyone is exposed to SARS-CoV-2 bound to become infected. We can get an estimate of how infectious a virus is by looking at a parameter called the secondary attack rate. The secondary attack rate is the proportion of people who become infected after coming into contact with an infected person. Therefore, a 100% secondary attack rate means that anyone who interacts with an infected person would also be infected.
As we might expect, the secondary attack rate will vary depending on the type of interaction. For example, the secondary attack rate of the household, and concentrating on individuals sharing the same household with the infected patient, tends to be higher than the secondary attack rate, including all types of interaction. Muge Cevik, a researcher in infectious diseases at the University of St. Andrews, divided on Twitter several published estimates of secondary attack rates. While the studies differed, the reported secondary assault rates in households were roughly between 10 and 20%, while the secondary attack rates considering all types of contacts were even lower.
An analysis of hundreds of COVID-19 cases in Shenzhen, as well as their close contacts, yielded a secondary household attack rate of 11.2%[1]. Similar analysis in Guangzhou showed a secondary attack of 17.1% among people sharing the same address as an infected person[2]. In a superspreading event in the US, a particularly high 53.3% secondary attack rate was calculated. These numbers mean that a person in contact with an infected patient will not necessarily be infected by the virus.
Third, even if a person becomes infected, death will not necessarily occur. The ratio of infection (IFR) compares the number of deaths with the overall number of infections. Determining the IFR is not easy because not all COVID-19 infections and COVID-19-related deaths are known in the absence of systematic testing and autopsy. Furthermore, it is easy to see that the chance of dying strongly depends on the demographics and the capacity and reactivity of the local health system. In addition, the IFR differs greatly between the population with the most vulnerable groups such as the elderly presenting a higher IFR. However, a team from the Pasteur Institute approved the IFR in France to 0.5%[3], which means that among 1000 infected persons, an average of 5 patients died. The Centers for Disease Control and Prevention in the US (CDC) has recently updated its epidemiological forecasts. Their best estimate yields an IFR for the US of 0.65%. The CDC further estimates that 40% of infections remain asymptomatic.
In general, this shows that exposure to SARS-CoV-2 does not give a 100% chance of infection, and being infected does not always result in death. Therefore, it is within expectations that most people who do not wear masks are still alive, and this cannot be used to draw conclusions about the usefulness or efficiency of masks.
Furthermore, masks not only protect themselves against infection, but they also reduce the risks of contamination of others. As a result, people with unintended faces indirectly benefit from a reduced virus transmission due to others wearing masks, analogous to the herd immunity effect. Indeed, Health Feedback previously stated that currently available scientific data support the fact that wearing masks reduces the risk of SARS-CoV-2 propagation by reducing respiratory droplets exhaling and inhaling. Analyzing the spread of COVID-19 in Wuhan, Italy and New York City, researchers found that face mask reduced the number of infections[4].
