Cervical cancer screening recommendations say HPV testing in combination with a Pap test, also known as a joint test, every five years, or just a Pap test every three years are still acceptable options, as not all labs have switched to primary HPV. tests.
The ACS last updated its guideline in 2012 and recommended starting screening at age 21. In a statement, the organization explained that the decision to increase the age for cervical cancer screening is due to new data suggesting that vaccination has led to a decrease in the rates of precancerous cervical changes, which are the cancer precursors.
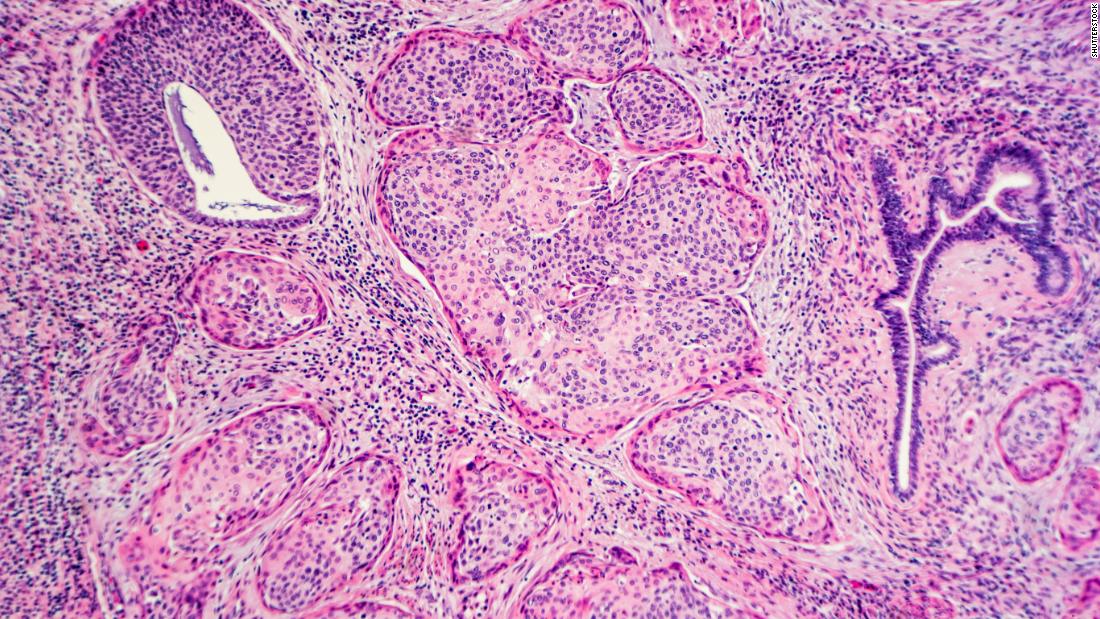
Cervical cancer is low in the 20-24 age group, and the numbers are expected to decrease as use of the vaccine increases, according to the ACS.
Debbie Saslow, managing director of HPV and GYN cancers for the ACS, said the new “simplified recommendations can improve compliance and reduce potential harm.”
“They are made possible by some important developments that have allowed us to transform our approach to cervical cancer screening, primarily a deeper understanding of the role of HPV and the development of tools to address it,” Saslow said in a press release.
People who are 65 years of age or older and who have had an adequate negative result on a previous exam may stop taking the exam. People with a hysterectomy may also suspend detection after two consecutive negative HPV tests, two negative co-tests, or three negative Pap tests performed in the past 10 years, with the most recent occurring in the last three to five years. . The ACS recommended that individuals without prior exam documentation continue to be screened until they meet this criteria.
According to the ACS, an HPV test is more accurate than a Pap test, and having one every five years can lower the risk of cervical cancer more effectively than a Pap test every three years.
“We estimate that, compared to the currently recommended cytology strategy (Pap test) alone starting at age 21 and switching to parenting at age 30, starting the primary HPV test at age 25 will avoid 13% more than cervical cancer and 7% more cervical cancer cancer deaths, “said Saslow. “Our model showed that we could do it with a 9% increase in follow-up procedures, but with 45% less testing required overall.”
All ACS guidelines on cancer detection are created by a group of 11 population doctors and health professionals, as well as a patient advocate.
Dr. Alexi Wright, director of gynecologic oncology and outcomes research at the Dana-Farber Dana-Farber Cancer Institute in Boston, said the ACS screening guidelines “are an important step in defining who should be screened and how to improve the results”.
“Cervical cancer could be eradicated within our lives in the United States if we do it right. It requires increasing HPV vaccination rates, regular screening, early diagnosis, and new therapies. But the most critical steps are to increase vaccination rates and detection. ”
.