The COVID-19 pandemic continues to cause tens of thousands of infections daily. Without a preventive, therapeutic, or antiviral vaccine, scientists are working at a hectic pace to find a solution. Now, a new study published on the prepress server bioRxiv * June 2020 shows that a candidate peak protein vaccine can induce neutralizing antibodies, T-cell antiviral responses, and protection against infection.
The SARS-CoV-2 S protein
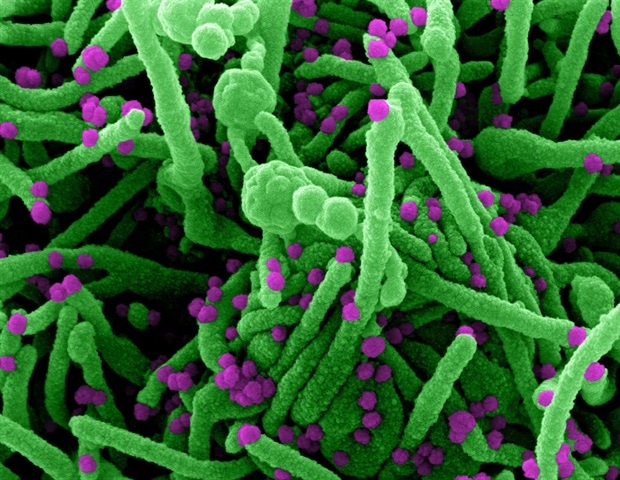
Coronavirus 2 of severe acute respiratory syndrome (SARS-CoV-2) is studded with spikes composed of glycoprotein. These are necessary for receptor binding, which triggers viral endocytosis followed by membrane fusion between the host cell and the virus. This allows the virus to enter the cytoplasm and replicate. It also stimulates the host’s immune response.
The spike glycoprotein is a fusion protein, an inactive precursor. At the S1 / S2 interface, the protein has a uniquely inserted polybasic furin cleavage site, not seen in the previous SARS-CoV. The binding of protein S, in the receptor binding domain (RBD), to the receptor of the host cell, causes the cleavage of the protein at the interface, generating the S2 subunit, which is conserved in all coronaviruses found in infections human, and the S1 cap which is more variable.
In addition to RBD, the S1 subunit also carries the N-terminal domain, while the S2 subunit carries the fusion peptide and other domains. Protein S is presented as a non-covalently associated trimeric protein. Like other fusion proteins, trimeric S protein undergoes a conformational change from its pre-conformation to the post-fusion conformation, after binding to the host cell receptor and proteolytic cleavage.
The effect of this structural change is exposure of the hydrophobic fusion peptide, which allows the virus to insert itself into the membrane of the host cell. Subsequent steps include alignment of the virus-host membrane, its fusion, and virus endocytosis, thereby entering the cytoplasm.
The study: immunization of animals with spike-based vaccine
The current study reports the development of a peak subunit vaccine based on the full-length peak protein of SARS-CoV-2. The stable prefusion protein S structure used in this vaccine was obtained by introducing a mutation at the furin cleavage site, whereby two proline residues were replaced in the center, making this site resistant to cleavage. . It shows a high affinity binding to the human ACE2 receptor.
The selected strain, labeled NVX-CoV2373, was thermostable, showed specific binding and high affinity for the receptor, and was stable under stressed conditions such as prolonged agitation, freeze-thaw cycles, and high temperatures.
The study used mice and non-human primates (NHP) to evaluate the vaccine strain for antigenicity and protection. This results in the blocking of antibodies against the human ACE2 receptor and the neutralization of antibodies against SARS-CoV-2. The vaccine was combined with a saponin-based Matrix-M adjuvant to assess the effect on immunogenicity.
High antibody titers
Mice were immunized with either a priming dose or a primer and booster, 14 days apart, at any of the four low doses (0.01 µg, 0.1 µg, 1 µg, and 10 µg) with 5 µg Matrix-M adjuvant.
Mice that received a dose in any of these doses developed high anti-S IgG titers 3-4 weeks after immunization. Those who received 10 μg also developed blocking and neutralizing antibodies within this period with a single priming dose.
When a booster dose was added, the highest IgG antibodies were present 7-16 days from the booster. Mice immunized with 1 µg or 10 µg of the adjuvant vaccine developed similar high antibody titers. At all doses, the priming / boosting program with the adjuvant vaccine caused high levels of blocking and neutralizing antibodies against the S protein.
The use of an adjuvant significantly improved the antibody titer: at doses of 0.1 µg, 1 µg, or 10 µg, mice receiving the adjuvant vaccine had higher titers than at the highest dose without adjuvant.
Higher B and T cell frequencies
The development of functional immunity depends on both components, the viral antigen and the adjuvant. The frequency of IFN-γ +, TNF-α + and IL-2 + that secrete CD4 + and CD8 + T cytokines was much higher in animals that received the adjuvant vaccine compared to the simple vaccine.
They also showed a higher frequency of multifunctional CD3 and CD8 T cells, T cells that secrete multiple cytokines, in those who received the adjuvant vaccine. The resulting CD4 T cell development was Th1 dominant or at least balanced between Th1 and other T cell phenotypes.
Immunization also induced the development of helper follicular T cells (Tfh) and center B germ cells in the spleen, which are essential to maintain the production of high affinity antibodies. They found that when combined with the adjuvant, the vaccine induced a more robust immune response in both groups of mammals, with the dominant role being played by T helper (Th) 1 cells, which involved B and T cells of the CD4 subtypes. and CD8.
The researchers comment: “These results indicate the possibility of a 10-fold or more dose savings provided by the Matrix-M adjuvant.”
Protection against infection
In mice infected with an adenovirus vector that expresses the human ACE2 receptor so that they can support replication of the SARS-CoV-2 strain, the results were surprising. The vaccine prevented the development of clinical infection, without the vaccine-associated improved respiratory disease (VAERD).
While unimmunized mice had 10,000 plaque-forming units (PFUs) of the virus per lung, those immunized with the vaccine alone, without adjuvant, had 1,000 copies per lung, and those that received the adjuvant vaccine had no detectable viral load.
In summary, at higher doses, mice immunized with a single priming dose showed no detectable virus. When a booster dose was also administered, all doses resulted in protection against infection, or at least 1 log reduction in load compared to non-immunized mice. The same trends were reflected with respect to weight loss in immunized versus non-immunized animals.

Representative histopathology of the lungs of 773 mice vaccinated with NVX-CoV2373 and Ad / CMV / hACE2 transduced mice challenged with SARS-CoV-2.
Non-human primates and sera from patients with COVID-19
In baboons, vaccine-induced anti-S IgG within 21 days of a single priming dose at all doses (1 µg, 5 µg, and 25 µg), while antibody titers increased by one log or more within two weeks after booster, again at all doses. When a simple vaccine without an adjuvant was used, the antibody was minimal or undetectable after the first and second doses.
Receptor blocking antibody levels were low after the first dose at all doses, but increased significantly after 1-2 weeks of booster. Neutralizing antibodies also increased in all doses after one dose and increased between 25 and 38 times after the second dose. However, the simple vaccine did not induce blocking or neutralization of antibodies.
Compared to antibody levels in recovered COVID-19 patients, titers were seven times higher in baboons than in the latter, along with 8-fold higher receptor binding and blocking antibodies.
Transcendence
These findings indicate the highly promising nature of this candidate for further development as a clinical vaccine. It is currently in phase 1 and 2 clinical trials to assess its safety and immunogenicity in humans.
*Important news
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and therefore should not be considered conclusive, guide clinical practice / health-related behavior, or be treated as established information.
.