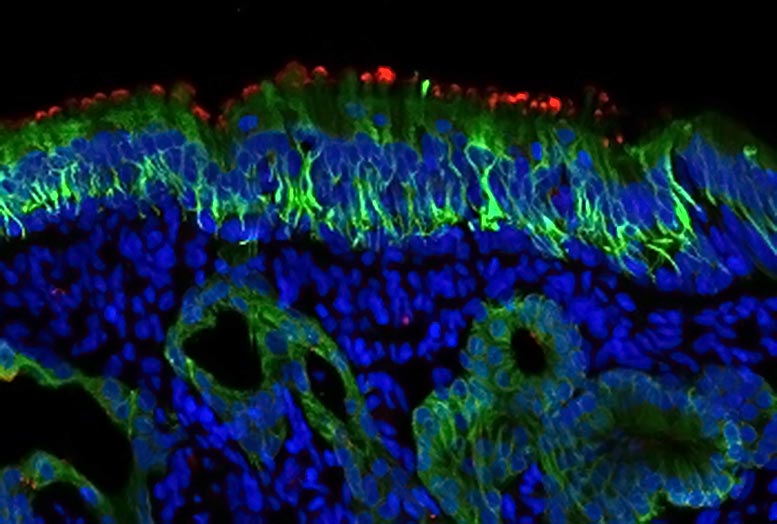

Red stain is ACE2. The green probe is cleavage of CK18, which is found in supporting cells and mucous glands. Credit: Mengfei Chen
Scientists at Johns Hopkins Medicine, experimenting with a small number of human cell samples, report that the ‘hook’ of cells used by SARS-CoV-2 to fix cells and infect cells is up to 700 times more prevalent in the oil factor supporting cells located inside the upper part of the nose than in the lining cells of the rest of the nose and windpipe that ‘ t leads to the lungs. These supporting cells are necessary for the function / development of cells with odor sensing.
The findings, from a preliminary study of cells containing both the nose and trachea, could advance the search for the best target for topical and local antiviral drugs to treat. COVID-19, and provides further clues as to why people with the virus sometimes lose their sense of smell.
A summary of the findings appears in a letter published on August 18, 2020, in the European Respiratory Journal.
“Smoking loss is associated with COVID-19, generally in the absence of other nasal symptoms, and our research may be looking for a definitive reason ahead of how and why this happens, and where we can best treat it. some treatments, ”says Andrew Lane, MD, professor of otolaryngology head and neck surgery, and director of the Department of Rhinology and Skull Base Surgery at Johns Hopkins University School of Medicine.
Lane’s medical practice focuses on people with nasal and sinus problems, who, he says, often lose their sense of smell – a condition called anosmia.
Scientists have known that SARS-CoV-2 binds to a biological hook on the surface of many human cells, called an angiotensin-converting enzyme 2 receptor (ACE2). The receptor runs in essential molecules.
In a bid to explore the ACE2 link to COVID-19 in more detail, Lane, Mengfei Chen, Ph.D., a research fellow in Lane’s lab at Johns Hopkins University School of Medicine, and others on his team looked closely at ACE2 levels in nasal tissue specimens of 19 adult men and women with chronic rhinosinusitis (inflammation of nasal tissue) and in tissues of a control group of four people who had nasal surgeries for problems other than sinusitis.
The researchers also studied tissue samples from the trachea of seven people who underwent surgery for abnormal trachea restriction.
Cells from children were not examined for this study, in part because they tend to have low ACE2 levels in the cells located in the nose, which may contribute to generally less severe disease among children who are infected with the SARS-CoV-2 virus. None of the study participants were diagnosed with COVID-19.
The scientists used a high-resolution imaging technique called confocal microscopy to produce very sharp images of cells that line the nasal and tracheal airways. They used fluorescent stains to identify ACE2 receptors.
They found high levels of ACE2 among nasal cells that provide structural support, called sustentacular cells. These cells are located in an area called the oil factor neuroepithelium, where odor-sensing neurons are found. The researchers say that this area of the nose can be particularly vulnerable to infection and may be the only infected site, even if there are no symptoms. Therefore, they encourage people to wear masks and wear them properly.
For the study, depending on the biopsy problem, cells in the olfactory neuroepithelium had a 200-fold to 700-fold increase in ACE 2 proteins compared to other samples from the nose and trachea. Because the cells with high levels of ACE2 are associated with odor sensing, the researchers suggest that infection of these cells may be the reason why some people with COVID-19 experience loss of smoke.
Two of seven trachea specimens had low levels of ACE2 receptors, and the proportion of those receptors was similar among student participants with and without chronic rhinosinusitis.
Because the cells that line the nose can prove a key entry point for SARS-CoV-2, Lane says there may be ways to target those particular cells with current antiviral drugs or other therapies directly to that area. .
The researchers plan to continue this research by examining COVID-19 infected tissue from the noses of humans to confirm if the SARS-CoV-2 virus is actually target cells in the nose.
###
Reference: “Increased ACE2 Expression in Olfactory Neuroepithelium: Implications for Anosmia and Upper Respiratory SARS-CoV-2 Entry and Replication” by Mengfei Chen, Wenjuan Shen, Nicholas R. Rowan, Heather Kulaga, Alexander Hillel, Murugappan Ramanathan Janan Raman Andrew P Lane, August 18, 2020, European Respiratory Journal.
DOI: 10.1183 / 13993003.01948-2020
Funding for the study was provided by the National Institutes of Health of the National Institute of Allergy and Infectious Diseases and National Institute of Deafness and Other Communication Storms (R01 AI132590, R01 DC016106.
Other scientists who contributed to the research include Wenjuan Shen, Nicholas Rowan, Heather Kulaga, Alexander Hillel and Murugappan Ramanathan Jr., of Johns Hopkins.