
[ad_1]
Worse still, it turns out that even for those who appear to have successfully recovered from COVID-19 infection and have recovered, the disease often does not end and the various symptoms that significantly impair quality of life do not disappear even after 6 months. .
If at the beginning of the global coronavirus pandemic, both doctors and researchers focused on the ways the virus spreads, its diagnostic potential, the main clinical signs of the disease, the frequency of complications, the search for treatment methods. (sadly unsuccessful) and the development of an effective vaccine, attention and the fact that the so-called recovery, when no virus is found in your body, even after retesting, does not mean that you will feel healthy.
Studies in many parts of the world have shown that after a coronavirus infection, between 40 and 90 percent of patients recover after discharge. patients have a variety of symptoms, which are described as postcovidial syndrome. “Post-COVID syndrome” – PCS).
Apparently, the symptoms of postcovidial syndrome could be classified as those that result from the direct exposure of the body to various body systems and the symptoms that result from a radically modified social environment and lifestyle and altered conventional stereotypes in a pandemic.

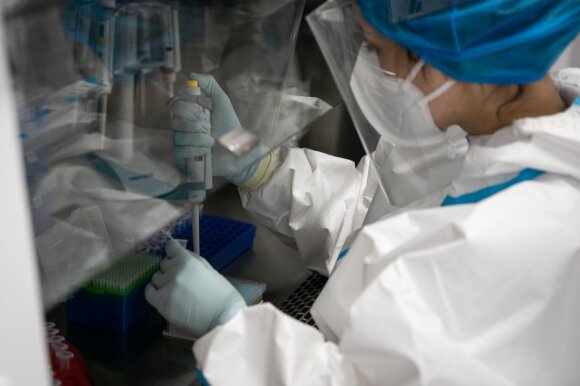
Associative photo.
One of the largest studies conducted by a group of Chinese researchers (C. Huang et al., 2021) found that in a study of 1,733 patients treated in hospitals 6 months after discharge from hospital, up to 63 percent. respondents indicated constant fatigue and muscle weakness. Up to 26% suffered from sleep disorders, 11% had no taste, 9% did not smell, and 7% noted movement problems. Signs of anxiety and depression were also found in most of the subjects studied.
By the way, a promising symptom was a significant decrease in the amount of antibodies compared to the active stage of the disease.
It is understood that the intensity of symptoms depends largely on how long the illness has elapsed. C. Carvalho-Schneider and her colleagues studied a group of 150 people with coronavirus infection last year. It was found that between 1 and 2 months after hospital discharge, 87 percent. As many as 59% of those surveyed experienced flu-like symptoms (headache, muscle and joint pain), and 59% reported taste and smell disorders. patients.
At 2 months, 2/3 of the people still noticed symptoms of dyspnea and asthenia. A survey of 120 people conducted by a group of French researchers (Garrigues et al., 2020) 110 days after discharge from hospital found that the main complaint was unmotivated fatigue – 55%, shortness of breath – 42%. cases. 30.8% complained of sleep disorders, 28% complained of decreased concentration. persons. Memory impairment was seen by up to 34 percent. investigated.
Since memory disorders can be very important, it is natural that in practically all countries GPs now advise their patients with a combat infection to write down telephone and bank card codes. Memory gradually recovers, but it takes not only a long time, but also special exercises.
The results obtained by colleagues from France, in accordance with data obtained by Italian researchers on 143 COVID-19 patients, are in complete agreement. The main complaints of the interviewed patients were weakness (53%), shortness of breath (43%), chest pain (22%) and joint pain (27%).
That weakness is the most commonly cited symptom and has also been confirmed by American researchers (MWTenforde et al., 2020). Incidentally, this study appears to be one of the most serious, as 274 patients with coronavirus infection were randomly selected from 14 centers.
I think some lab tests are important enough in terms of post-ovid syndrome. This syndrome has been shown to be characterized by lymphopenia (low lymphocyte counts) and high levels of ferritin and D-dimers.
Lymphopenia is easy to explain because a significant decrease in the amount of antibodies (insufficient immune response to the virus) is often found in this syndrome. High levels of ferritin occur in the presence of inflammation, autoimmune reactions. D-dimers are one of the most sensitive indicators of the coagulation system.
An increase in D-dimers indicates that clots can form. After all, we are very aware that in the case of coronavirus infection, vascular thrombosis occurs, so controlling this indicator becomes very important in the daily work of a family doctor.
With regard to post-covidium syndrome, it should be noted that this syndrome affects the quality of life of the patient, but the good news is that radiological and spirometric examinations of the lungs are only 25% of patients showing weakly expressed negative changes. Consequently, the lung tissue recovers after the coronavirus infection and other unpleasant symptoms of the patient’s suffering gradually disappear. But it takes time.
It is strictly forbidden to use the information published by DELFI on other websites, in the media or elsewhere, or to distribute our material in any way without consent, and if consent has been obtained, it is necessary to cite DELFI as the source.
[ad_2]