[ad_1]
– Laboratory samples can also be infected. Could you explain a bit how this can happen?
– A living person is more dangerous, especially when you interact with him, when he speaks, when he undergoes certain procedures. At that time, the samples that are analyzed in the laboratory are the same environment in which the virus lives. Therefore, the danger is the same, especially when the sample is opened, it moves.
– The purpose of this conversation of ours is to explain a little to people the differences between certain research methods and other medical terms. Do you notice that people still confuse various medical terms related to the coronavirus? Or is it the same in the media?
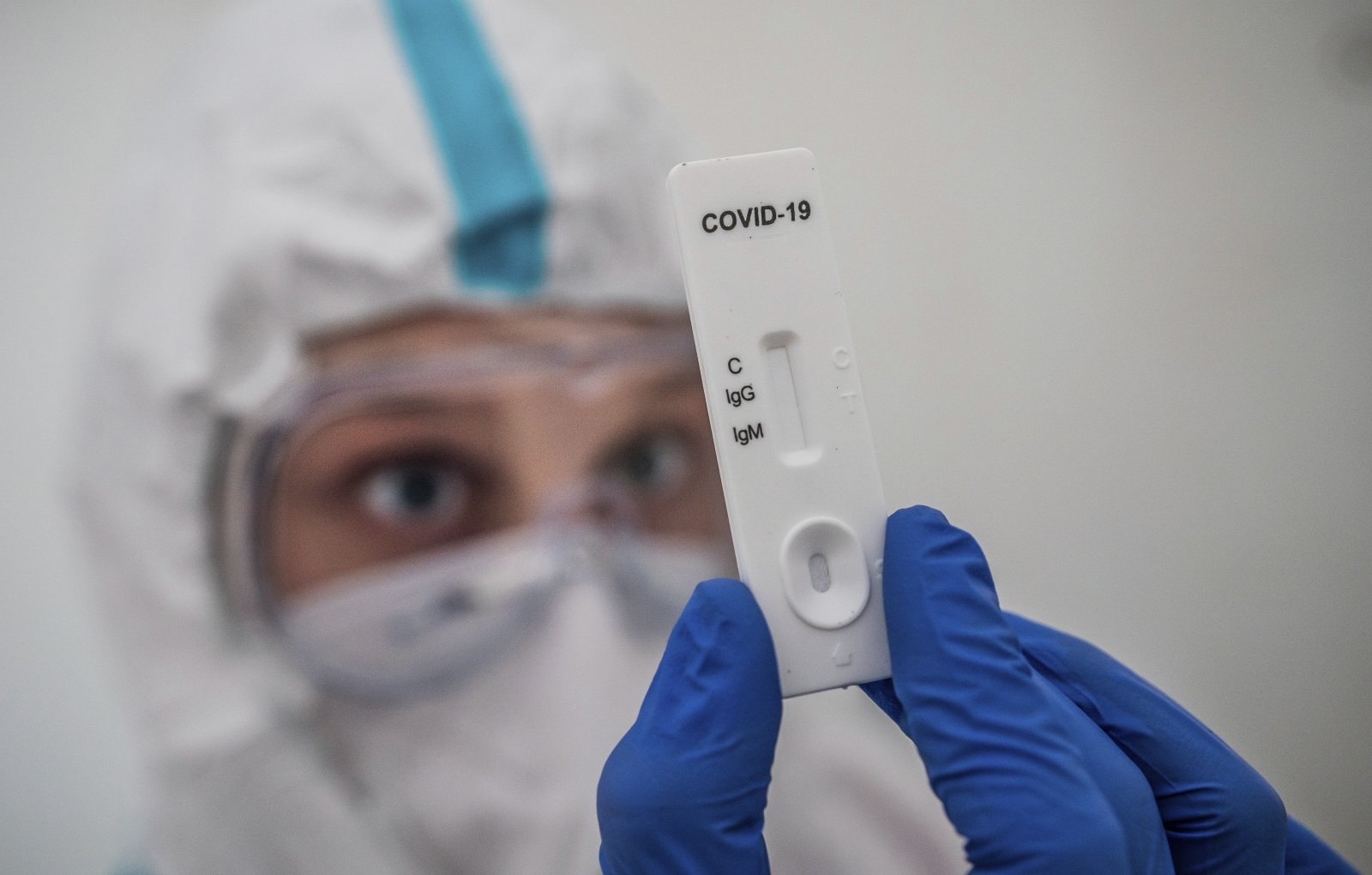
– Everything happens. It is important to distinguish between 3 main research methods. PCR is used to identify viral genetic material. Antigen test: An antigen is part of the structure of a virus that the body accepts as foreign. Before that, the antibodies are made. Therefore, we can identify genetic, structural and antibodies already created by man.

– It was recently announced that the government will encourage companies to perform rapid antigen tests on their employees starting in February. Perhaps we can point out what tests are currently available in Lithuania?
– The so-called gold standard: the PCR method has been used in Lithuania since spring. Identify the genetic material of the virus. Usually 3 genes are studied, sometimes limited to 2 genes. It is a substance that codes for individual viral proteins. They are antigens. When a viral cell enters the human body, it is recognized as a foreign substance and our body begins to produce antibodies. So, there are 3 tests: the first is the detection of genes, the second that came before is the test for the detection of antibodies; These are the substances that our body produces to fight the virus. And the third one we look forward to is the antigen test.
– Let’s talk about everyone in more detail. The PCR test is the one used first. How long can we get an answer after taking this test? This is probably the main difference between rapid and PCR tests.
– As is known today, the highest probability of detecting a virus is after 5-7 days of infection. Of course, that time interval can be longer and a detectable virus can only form within 14 days of contact. However, if, for example, you had contact with COVID-19 yesterday and are investigating today, you will not find anything. Each studio has its own time. The situation is similar with the antigen test, but in this case the time is not calculated from the contact but from the onset of symptoms. When the first symptoms of COVID-19 appear, 5 or at most 7 days later is the right time to perform the test. Not by contact, but by the appearance of symptoms. And the antibodies appear later, about 2 weeks after the onset of symptoms, and can be detected both by rapid tests and in the laboratory.

– Rapid antibody tests are available from spring. How reliable are they?
– Basically it depends on the manufacturer. But the ones that are bought across the country, as tests have shown, are reliable and can be trusted.
– If a person undergoes such a test and tests positive, but there are no symptoms, what to do for them? Do you perform a PCR test?
– If antibodies have already been detected, there is no point in performing a PCR test. This indicates that there has been contact with the virus, that it may have disappeared completely without symptoms, or that perhaps even minor symptoms have not been addressed. However, there are quite a few people who have antibodies but do not know they were sick or do not know when they had contact.
– Before the interview, I looked at the tests offered by private laboratories. One of them was a rapid PCR test, in which you get a response within 1.5 to 5 hours. Is this the rapid antigen test?
– The traditional post-sampling PCR test consists of 2 parts. Viral ribonucleic acid is isolated first. The second stage of the study is the multiplication of secreted acids. If they multiply, it is concluded that the virus is present in the body. The duration of the study is 3 to 6 hours. Rapid PCR assays combined the two steps at one site, resulting in a much faster response. But basically the same research.
– What is the difference between the accuracy of rapid PCR tests and routine tests?
– They are identical in their precision.

COVID-19
– Or kaina?
– And the price varies from 2 to 10 times in favor of high speed. Unfortunately, rapid tests are not on the market as much as they should be. And Lithuania is not an exceptional country, it is a problem for the whole world. As a result, the main site for rapid PCR testing is the admission rooms of large clinics, which house the most difficult patients.
– There is a lot of talk right now about rapid antigen tests. As much as you had to interact with the business, the opportunity to purchase such tests would be a huge relief. Do you need a special worker to make them? Or maybe you can do it yourself?
– The rapid antigen test itself is not difficult to obtain, it can be performed by any personal health professional without very special training. However, an important step is sampling because, as in the PCR assay, it is taken from the nasopharynx. This should be the main focus, as it is important to have a quality sample. So on the one hand, I very much agree that when there is some risk, it would be a great tool. But the sample must be taken by a trained person. To obtain the result, this test does not need a laboratory; It can be done where the patient is, it is not necessary to go anywhere. However, safeguards still need to be followed.
Coronavirus
– Another test is for antibodies. Some have enough even after 9 months, others go away much faster. Do we know why they last longer in some and less in others?
– Unfortunately, no one knows yet. What is already known is that antibodies against one of the viral proteins persist only for about 3-4 months. At that point, the antibodies that are formed against the needle protein persist for much longer. Antibodies against needle protein are currently the most studied, as they are likely to survive the longest, whether you’ve been sick or vaccinated.
– Some countries have chosen to survey the majority of the population to control a pandemic. Is this real? Would that help control the pandemic?
– I think it also depends on the size of the country and its capacity. The bigger the country, the harder it is to imagine how it would be implemented. However, this would only be a snapshot cross section, data that reflects a certain time interval.
– Could it happen that in the future we go to the pharmacy, buy a test, do it and find out if we are sick or not?
– I think it may be real. The first methods of this type already exist, although they have not yet been sufficiently explored. But I think there will be such an opportunity in the future.
It is strictly prohibited to use the information published by DELFI on other websites, in the media or elsewhere, or to distribute our material in any way without consent, and if consent has been obtained, it is necessary to indicate DELFI as the source. .
[ad_2]