[ad_1]
The professor spoke about this and other topics related to the COVID-19 vaccine in a remote talk-discussion “COVID-19 vaccines: challenges and technological innovations”.
According to A.Žvirblienė, the biggest challenge we face during the pandemic is its scale.
It takes a large number of people who have acquired immunity to control it.
Of course, he said, herd immunity could be achieved even if most people just got sick, but that would require a large number of deaths.
Therefore, vaccination is the main weapon against a pandemic.
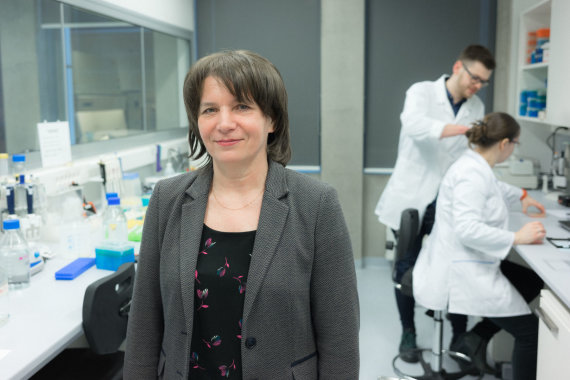
Photo by E.Kurauskas / Dr. Aurelija Žvirblienė
With 70 percent. populations will guarantee herd immunity?
On Tuesday, President Gitanas Nausėda announced an ambitious goal: get 70% vaccinated in midsummer. populations and thus achieve herd immunity.
However, the question arose as to whether this number of people was sufficient when as many as 90 to 95 percent had previously been vaccinated against other viruses. population of the country.
In response, Professor A.Žvirblienė emphasized that, first of all, it is necessary to pay attention to the rate of reproduction of the virus.
This means calculating how many people around you can be infected with the virus from a single resident.
According to her, this rate of coronavirus is lower than, for example, the measles virus, so we can achieve herd immunity by vaccinating a smaller population.

Photo by Rokas Lukoševičius / 15min / Afternoon of winter fun in Vilnius
On the other hand, he pointed out, 70 percent. it is a more theoretical than practical indicator.
“The virus is mutating and becoming more contagious, and the percentage of the population may need to be higher.
In general, 70 percent. It is a more theoretical figure, it has been published since the beginning of the pandemic. Of course, this would significantly stop the spread of the virus, but there is also the fact that not all age groups have been included in clinical trials and therefore cannot receive vaccines, which is an important part of society. . Wanting not wanting would not be able to reach 95%. vaccination level.
“We will see in other countries, such as Israel, which has vaccinated almost a third of the population, that 70% will soon be there, and we will see from that real world data if such an assumption has come true”, the professor. explained.
The virus mutates and becomes more contagious, perhaps the percentage of the population should be higher.
How often should you get vaccinated?
Professor A.Žvirblienė highlighted that the question of vaccination frequency is one that can only be answered after a longer period of time.
Currently, he said, data is only collected from the third phase of clinical trials.
Therefore, volunteers who were the first to receive a dose of COVID-19 are continuously monitored to collect additional data.
“We may not have to get vaccinated every season, perhaps there will be a longer response. But it is not yet clear,” he said.
However, it should be noted that immunity can also develop against the background of COVID-19 disease.
The professor pointed out that talking about immunity thus acquired was avoided for some time because no one could guarantee or provide evidence that protection would last longer after illness.
However, the results of several studies were published before Christmas showing that immunity was developing.
People who had antibodies were ten times more protected from infection.
“The study showed that about half a year after illness, people who had antibodies, no matter how much, were ten times more protected against infection than those who did not have antibodies,” he said.
According to Professor A.Žvirblienė, this means that the disease creates protection similar to that of vaccination.
“According to the data now available, the period is similar. Therefore, there is a recommendation for people who are ill, even a few months ago, and have antibodies, not to get vaccinated,” explained the researcher.
What to do for people with autoimmune diseases?
For certain groups of people, the vaccine may not work due to an autoimmune reaction.
According to A.Žvirblienė, it is necessary to ask questions about the effect of vaccines in these populations, because there is a certain risk.
However, the vaccine, he said, is still worth it because the viral infection itself is often more dangerous for them than it is for the average person.
“Infectious diseases are usually like trigeriai autoimmune diseases, ”he noted.
“There is such a choice between the two evils, the greater and the less.
Be that as it may, the vaccine is probably a lesser evil than a disease. But we must wait for these data until they are available in the long term, “said the professor during the discussion.
Can vaccinated people carry the virus?
The researcher also noted that even vaccinated people cannot try to circumvent coronavirus restrictions because they can carry the virus even if they don’t know it.
And this is very dangerous for the population at risk.
“From clinical trials, there is no unequivocal answer that vaccination actually protects against transmission of the virus. <...> We do not have 100% data that all vaccinated people are completely protected from asymptomatic or virus-carrying infections ”, emphasized A.Žvirblienė.
Therefore, it argues that the same safety requirements must be met until all groups at risk have been vaccinated, both the vaccinated populations and those exposed to coronavir.
“Until they are vaccinated and thus protect themselves, we must also try not to spread the virus. Because we can distribute it without knowing it, ”he said.

Photo by Lukas Balandis / 15min / Aurelija Žvirblienė
Is it worth worrying about?
“These processes have been greatly accelerated, but no essential stage has been missed,” said A. Žvirblienė, speaking about vaccine development and concerns about their safety.
The manufacturers of vaccines approved by the European Medicines Agency, without exception, had to take the appropriate measures: firstly, testing the vaccines in animals, from the smallest such as mice to studies in monkeys.
After this stage, the vaccine manufacturers had to conduct multi-phase clinical trials.
These, according to the researcher, are made initially with several volunteers, then with hundreds and finally with tens of thousands of people.
“Those vaccines have passed all stages and phase III clinical trials have been completed,” he said.
These processes were greatly accelerated, but no essential stage was missed.
Questions still unanswered
During the talk, the professor emphasized that there is a lot of positive knowledge related to the COVID-19 vaccine: we have effective vaccines, we have new technological platforms, such as RNA vaccines, new vaccines have been developed in less than a year.
According to her, these new technologies, if finally successful, could be used more and more in the future.
Furthermore, new challenges, such as low-temperature vaccine transport, are being addressed fairly quickly.
And with the introduction of mass vaccination, data on the efficacy and safety of vaccines will become increasingly available.
However, we still don’t have some answers.
“There are still some unanswered questions: If the mutations will not change the effectiveness of vaccines, we don’t have long-term data on how long the immune response lasts, we only have data on clinical trials, which started in the summer.” so we have about half a year.
When very old people are vaccinated, such as those over 80 years old, their immune systems do not respond as well to immune antigens. Here, too, there may not be as much efficiency as in youth.
Children and pregnant women were not included in the clinical trials, so this data has not yet been collected to vaccinate these groups, ”he said, answering unanswered questions and challenges.
What vaccines are being developed and how are they different?
According to A.Žvirblienė, a paradoxical situation has emerged at this time, as traditional vaccine development formats lag far behind innovative ones.
An example is an inactivated virus vaccine.
Currently, only one manufacturer of this type of coronavirus vaccine is being developed in Europe.
“They are far behind in clinical trials and their record is likely to be the most recent,” he said.
Currently, less popular and more traditional protein vaccines using viral protein with adjuvants are also available.
These vaccines are currently manufactured by the pharmaceutical company Sanofi and the biotechnology company Novavax.
However, according to A.Žvirblienė, his research is also lagging behind in time.
The most advanced vaccines are based on innovative technologies.
Moderna and Pfizer are informational RNA-based vaccine development technologies that encode a viral protein. These vaccines are administered to the Lithuanian population.
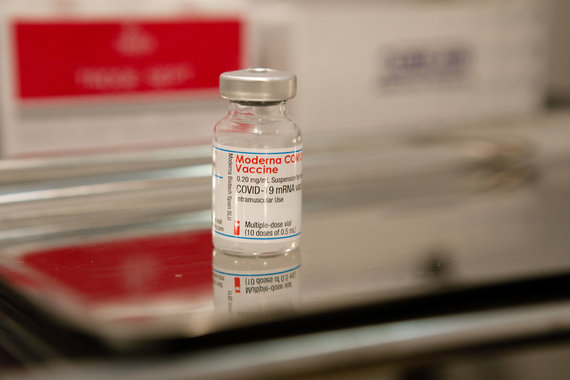
Erik Ovcharenko / 15min photo / Vaccination point installed in the old post office
“Until now, these types of vaccines have not been used in the market, but of course those vaccines have not been developed in a blank space, the technology existed before. But when the need arose, they adapted very quickly to develop a vaccine, “explained the researcher.
Although there were threats that embryonic cells would be used to develop vaccines, A. Žvirblienė said there was no reason for such fear.
“The special feature of these vaccines is that they are developed completely artificially. <...> therefore, there are no cells, no viruses, only artificial technologies, ”he noted.
Researchers from the University of Oxford and the pharmaceutical company Astra Zeneca have used another format to develop a vaccine based on DNA viruses.
Non-human viruses are used in the development of this vaccine.
No cells, no viruses, just artificial technology.
Because the technology is simpler, A.Žvirblienė stated, it is possible to transport vaccines based on it under milder conditions, deep freezing is not required.
SEE ALSO: Coronavirus Vaccines and Mutations: Can the virus change so that vaccines become ineffective?
Currently, two different vaccines are used in Lithuania, i.e. companies in general The vaccine is being developed by Pfizer and BioNTech and manufactured by Moderna.
According to data from the Department of Statistics on Thursday, January 21, 56,358 people have already been vaccinated with the first vaccine in Lithuania, that is, slightly more than 2 percent. populations.
Just over 8,000 people received the second vaccine. people.
[ad_2]