[ad_1]
During the conversation, J. Grigaitienė repeated the phrase “a lot”. This laconic phrase hides an incalculable number of patients who have been infected with the coronavirus and who have died from its complications. He also distinguishes the interlocutor’s experience from his colleagues in Lithuania: in London, where the quarantine was announced later than in our country, the coronavirus hit much harder than in Lithuania in general.
“What scared me the most personally was not the fact of death itself, but the fact that people went through all that long hospitalization alone and died alone, without a family, surrounded by space suits. Therefore, the medical staff, especially the nurses, tried not to forget primary human care alongside the heavy workload: they made video calls with their families and tried to make the experience a little bit. We try to take recovery patients from Intensive Care to the field for at least a short time to see the sun; This will probably remain one of the most beautiful memories, “said the interlocutor.
We invite you to read the entire conversation with the anesthesiology and resuscitation resident of the Kaunas clinics. Grigaitien Jurgitame.

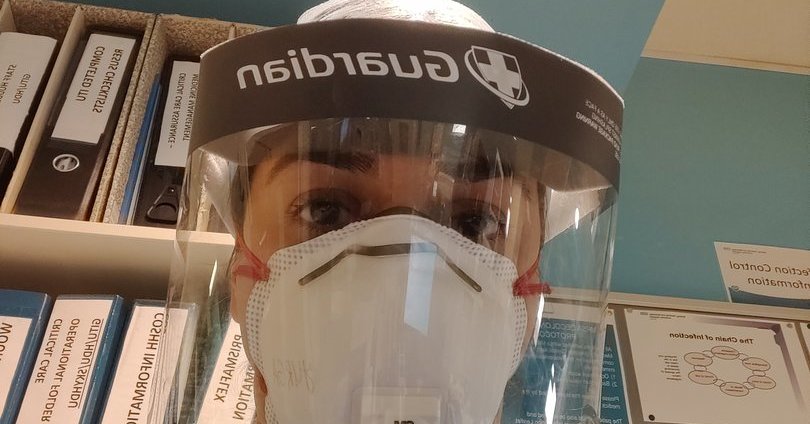
Personal photo / Resident of Anesthesiology-Reanimatology Jurgita Grigaitienė
– Tell us about yourself: how long have you been in medicine, what have you been doing in Lithuania and how have you found yourself in one of the largest hospitals in London?
– I am a fourth year resident of resuscitation with anesthesiology, I am currently completing a residency at Kaunas clinics. I have been in medicine for ten years, but my clinical experience is four years. 2019 In April, I went to London for a one-year internship in the Intensive Care Unit at Queen’s University Hospital, London. I came back just a couple of weeks ago, a little later than planned. I am in self-isolation during our conversation.
– During the internship in London, a pandemic hit you. Perhaps you can tell us about that period, working in resuscitation at Queen’s University Hospital?
As you know, the London coronavirus has been covered a lot. Our hospital is in East London, and the hospitals here have been hit by the pandemic. As it happened, she was one of those treatment facilities that had to withstand the highest flow of patients.
– What did that “bigger stream” actually look like?
– The first case in intensive care was confirmed in the first fortnight of March. Since we had already received reports of coronavirus cases at other hospitals, we knew we would be there. Now I think we were well prepared then: increasing the number of beds in the Intensive Care Unit, bringing in the machines. Training for staff from other departments began because we realized that if there were more patients, more staff would be needed. For example, nurses. Intensive care nursing is specific, so in a short time it was necessary to teach people who worked in other departments the basic things they would have to face. While they worked, they obviously always had a more experienced person nearby. But since there were actually many patients, it was necessary to have staff who were unfamiliar with and working on resuscitation.
– Do you remember how you felt then? What emotions were the strongest?
– There was definitely no certainty (laughs – aut. Past). The most memorable was the uncertainty. You can prepare everything you want, know what you need, but when the disease comes, there are still many questions. Mainly because the disease itself is completely new. We have seen other coronaviruses, but this one is different. We did not fully know what systems of the body are damaging, how to treat the infected, what to do and what not. At first, we both worked and learned from our mistakes.
At first, we both worked and learned from our mistakes.
It was difficult due to the constant need to be with all the safeguards. In our department, the greatest contact with the infected, so protective equipment had to always be used. It bothered me not only physically but also emotionally.
– How much did your turn interfere at the busiest time? Maybe it was like you hadn’t left the hospital at all?
– In our department, the shifts, as before the quarantine at 12 o’clock, were kept that way. It is true that, although the total number of working hours did not change, they were distributed differently over time. T.y. New work schedules have emerged for the March period. A much larger group of doctors worked, we used anesthesiologists to help and there was more turnover.
– Were you able to rest when you got home? Or maybe, while protecting the cohabitants, she moved to another place at that time?
– He lived alone in dormitories for medical personnel near the hospital. I am very happy to have a separate room. My whole family stayed in Lithuania. It really made me feel calmer. I know that for other employees who had to return to their families, that really stressed them out. Especially at the beginning. It used to be that the doctor, after completing his shift, bathes in the hospital, changes his clothes, returns home, washes again, and only then communicates with the family.
– What was the most difficult moment or situation that required you the most?
– At the end of March, when the most intense work was in our room, due to the greater flow of patients, the constant calls were very tiring. In our hospital, there were such tasks that the attending physician consulted other departments by phone. The doctor working in the intensive care unit also consults other units on the designated day. These were the days when my phone kept ringing full time: 10 calls a day. It is difficult because he consults himself without knowing the disease well, he does not know how quickly the condition will worsen for that person. That uncertainty and workload, only occasionally increased, was the most debilitating experience.
And in general, the most difficult part of that period would be to see the rapidly changing condition of infected patients change. He used to go see the patient, everything seems fine for him. And after an hour they invite you because the same person is seriously ill …
He used to go see the patient, everything seems fine for him. And after an hour they invite you because the same person is seriously ill …
– What motivated and strengthened the fight against strangers and other major or minor challenges of the coronavirus?
– Maybe it helped that we were open with the patients. We have said that, based on current evidence, what we know are basically two ways to help them: a non-invasive ventilation mask and a translation in the abdomen. We explain that it will or will not help. If that doesn’t work, mechanical ventilation will be needed. If necessary, the patient’s outcome will likely be poor. They knew what we could do and how it would not be in our hands. I think everyone has realized that we are not gods and that we cannot do more than we know and do now.
I think everyone has realized that we are not gods and that we cannot do more than we know and do now.
– Deaths are inevitable while working in the Intensive Care Unit. However, during the coronavirus pandemic, there were many more than before. How did you manage to endure all this?
– There have been many deaths from Covid-19. Although we always see them in the Intensive Care Unit, we are never used to it. Clearly, learn to work with it. No longer surprising, not accepting in person. But in this case, there were many deaths, because there were also many sick people.
For me personally, what was most terrible was not the fact of death itself, but the fact that people went through all that long hospitalization alone and died alone, without a family (due to very limited assistance), surrounded by people dressed in space suits. As a result, medical staff, especially nurses, tried to take basic human care into account, in addition to the heavy workload, made video calls with families, and tried to make the experience a little bit. We tried to take the patients recovering from Intensive Care to the field for a short time to see the sun; this will probably remain one of the most beautiful memories.
– It is a truly wonderful memory, as well as proof of how important even small things are. Do I understand correctly that it was easier to endure the most difficult moments due to good relationships with colleagues?
– You know how it happens: when there are problems, people come together. Even if there was some anger in the team before, everything was forgotten. We all had a common goal: to survive the first wave, and we helped each other a lot.
– You mentioned that while working in the hospital, you did not feel much anxiety and were happy that the husband and other family members lived apart from you in Lithuania. And how did your loved ones and friends react by working in very extreme conditions?
– My voice may sound calm, although there was anxiety (laughs – aut. Past). But you know how it happens: you endure that cold shower, that first wave of uncertainty, and then you accept the need to adapt as quickly as possible. I think we will soon reconcile with the support of the team.
The family, of course, was excited. We call everyone every day, despite the time difference: it’s two hours later in Lithuania, so when I finished the shift, it was sometimes already around midnight. But they were still waiting, asking if everything was okay. Understood if I didn’t want to tell you what happened in the hospital that day.
– Were there many moments that you did not want to count?
– There was (laughs – aut. Past). It took you time to think about what and how much to count. There are things you can say to a colleague because you know they will really understand him. But you don’t necessarily want to tell your family without filtering everything so you don’t get scared. You must first think for yourself and then count it.
– In a word, you selected information and made your loved ones think that it is better than it really is.
– yeah But on the other hand, I wanted to show the situation as it is. Because in both Lithuania and England there were those who denied the threat of the virus, the need for quarantine. Once there was quarantine in Lithuania, there was still freedom of movement in England. The quarantine was announced later.
– How did you and your medical colleagues react to such delays and denials of the threat of a pandemic? After all, were there patients with coronavirus already in the hospital?
– It is very easy to condemn, fire the fools. It seems natural to me that people react differently. When you tell me that you need everyone to feel at home, it is unclear how long, I realize that for some, the natural reaction is to resist. But of course we were angry at those who did not protect themselves or others. Especially in those who do not protect others. After the introduction of quarantine, everyone has already seen that it works.
– What is the situation at the Queen’s Hospital now, after the first wave of coronavirus has subsided? Everything goes back to normal?
– Just before I left, I was much calmer than during rush hour. The coronavirus wave is abruptly decreasing. What has changed in our country and, I think, in other hospitals: before the peak that we increase the Intensive Care Unit, it will continue to be bigger. The number of beds in intensive care units is increasing across London, i. safeguards more patients as well as staff. Of course, this is also related to the second expected coronavirus wave. No one knows what size and when it will be. Everyone understands that for a year, maybe even two, we will have to live with this disease. When I went to Queen’s Hospital, I left him changing and planning how to protect patients who come to scheduled services so they don’t get infected. Because some patients (infected with coronavirus – aut. Past) who were found in the Intensive Care Unit while still working are still sleeping. They are in the Intensive Care Unit for an infinitely long time. Weeks, months … Covid-19 is an infinitely long illness. In the last days of my job, I was still treating some of the patients I had slept with a month and a half ago.
Covid-19 is an infinitely long disease. In the last days of my job, I was still treating some of the patients I had slept with a month and a half ago.
– What experience was memorized as the brightest?
– I reiterate: it is a sample of how fast we can mobilize, we know how to support each other. It is just phenomenal. It used to be that when he saw in his eyes (because everything else was hiding protective clothing) that he was tired, a colleague offered him to go have a cup of tea. It’s really amazing when other people make sure you don’t forget to take care of yourself.
Another moment: patients. If someone from the Intensive Care Unit was prescribed, no matter how he didn’t treat it, everyone knew his name, everything about him. You are happy with each recovery.
If a patient was discharged from the Intensive Care Unit, everyone knew his first and last name, everything about him. You are happy with each recovery.
Covid-19 recovery is slow. But there were healers. Of course, it should be understood that the “healed” have healed so much that they can be discharged from the Intensive Care Unit. They will still need long-term rehabilitation, not to mention that they will return to a much lower functional level than before the disease. But these problems are for the future. We are glad that they survived.

Personal photo / According to J. Grigaitienė, the support of colleagues was especially important when they worked at Queen’s Hospital in London.
– During the quarantine in Lithuania, doctors felt a strong sense of public support: various campaigns were organized, food was delivered to hospitals, etc. Did you feel that support in London?
– The English are very respectful of their health system. We also feel support during the pandemic. There were as many public actions as in Lithuania. I even told my colleagues at the hospital to see how the Lithuanians are doing. However, we also feel support: starting with food twice a day; They also had hand creams. It seems a little small, but when you wash your hands 50 times a day, they really crack and sometimes the cream can save you from pain. There were other things like applause. I don’t know who proposed that campaign, but in the afternoon during a certain hour everyone applauded the personnel of the health care system. The medical staff were also able to take a free taxi.
Definitely nice, support is important. However, I don’t think doctors were heroes, as it is sometimes said somewhere. I think we were all beaten. Our job is to treat others to ensure the functioning of other chains. Everything worthy of respect.
– What would you and your colleagues who work in medical institutions like?
– I wish what I’m already doing now. As I have time, I had to isolate myself for two weeks when I returned to England, I calmly reflect on everything and try to understand the lessons learned from that period. The virus hit us without preparation, together we resisted the first wave. It should be understood that this is neither the first nor the last virus. There will be many more. Therefore, it is necessary to keep those lessons for future generations, when it will be necessary to mobilize very quickly, to adapt to an extremely changing situation.
It should be understood that this is neither the first nor the last virus. There will be many more. Therefore, those lessons must be maintained for future generations.
And I wish my colleagues collegiality and teamwork. Lithuania has not received a coronavirus hit like the one in England, and thank goodness. But when that hit hits, it is extremely important to be a pillar for your colleague. Neither stick your finger in mistakes, but support others psychologically as much as possible.
– What will you do first after self-isolation (there was one day left during the conversation – aut. Past)?
– I will go to Klaipeda, to my family. The man is currently on vacation, spending time with me. Without that, it would be more difficult! And on Monday I will go to work at the Kaunas clinics.
– Thanks for chatting!
[ad_2]