[ad_1]
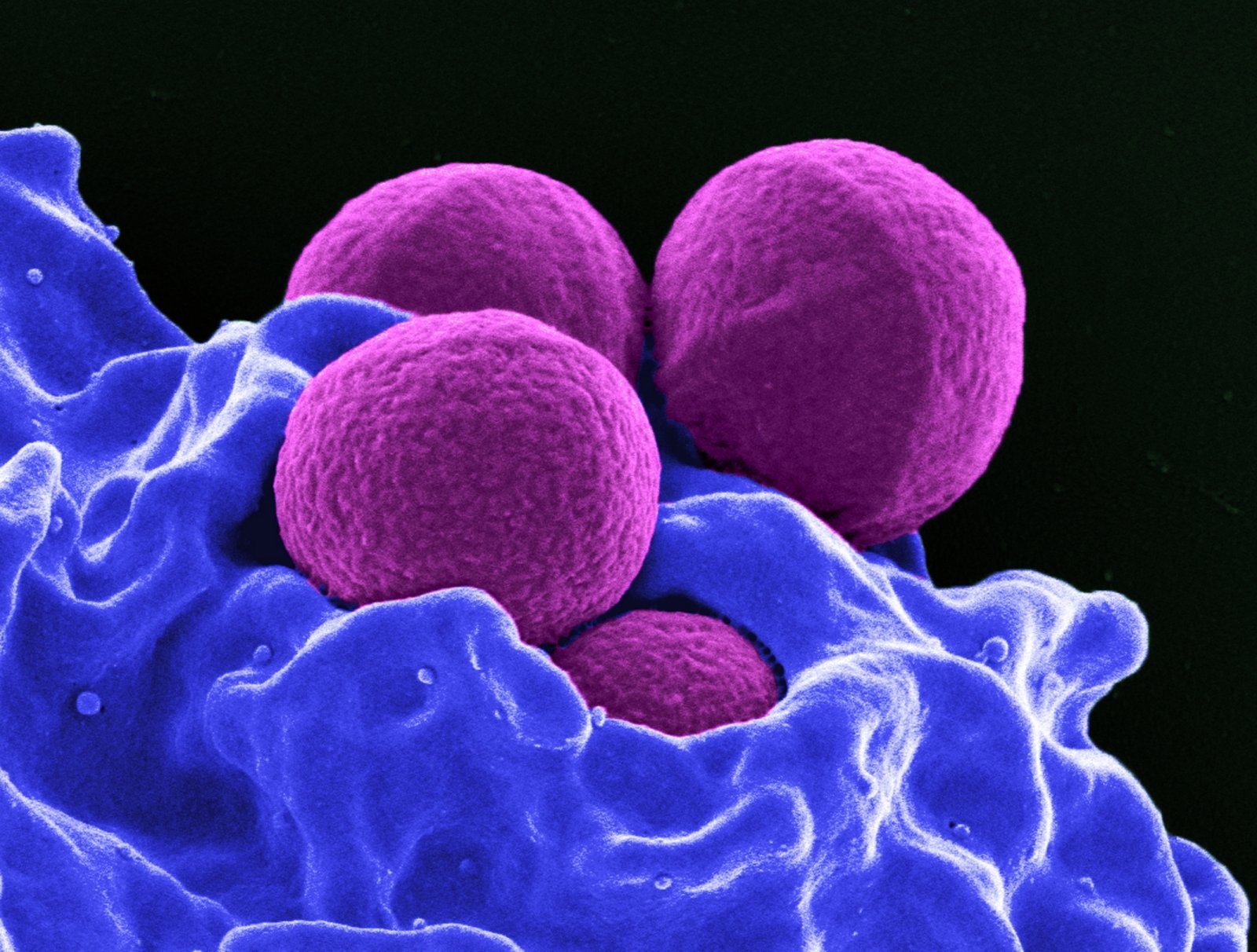
Antibiotic resistant bacteria no longer receive as much attention as COVID-19 because the diseases they cause spread slowly and steadily, instead of covering the entire world in almost an instant. However, such bacteria could become a threat at the COVID-19 level, experts warn. And it is already happening.
According to the US Centers for Disease Control and Prevention, nearly three million Americans are diagnosed with an antibiotic-resistant bacterial infection each year. Of these, about 35 thousand. go dead.
Around 700,000 people worldwide die from these infections each year. people. The World Health Organization estimates that if current trends continue, about 10 million people could die from antibiotic-resistant infections by 2050. people.
The overuse of antibiotics, their overuse in livestock, and other factors have made a number of different bacterial infections, including some types of gonorrhea, tuberculosis, and salmonellosis, extremely difficult to treat and sometimes incurable. This is because a small percentage of these bacteria that survive antibiotics change and multiply, thus developing resistance.
Worldwide, 230,000 people die each year from antibiotic-resistant tuberculosis alone. people.
“Bacterial infections are more and more likely to be very difficult to treat and incurable bacterial infections are very bad. Incurable bacterial infections do a lot of damage. They kill people, ”said Sarah Fortune, professor of immunology and infectious diseases at Harvard University.
Steffanie Strathdee, a professor of medicine at the University of California, says the threat is not being addressed enough.
“Unlike the coronavirus, which appeared and spread suddenly, the superbug crisis has been going on for some time,” he said. – You already have a pandemic. This is already a global crisis and the situation is even worse in the context of the coronavirus. “
Tom Frieden, former director of the US Centers for Disease Control and Prevention, said the US government needed a more aggressive and multifaceted approach to combat what he called “nightmare bacteria.” He said the medical community must pay special attention to how infectious diseases spread in hospitals.
“I have absolutely no doubt that in 20-40 years, we will look at the healthcare system and what was implemented in 2020 and shake our heads on how they could have allowed such a large number of infections to spread in care facilities medical, ”he said. “We are not even close to where we should be in terms of infection prevention and control.”
A “dysfunctional” public health system makes it difficult to solve the problem
Much of the attention and resources that bacteria should receive is now devoted to fighting the coronavirus, Strathdee said. In this regard, therefore, the coronavirus pandemic contributes to the problem of antibiotic-resistant bacteria.
In July, the WHO called for more caution when prescribing antibiotics to coronavirus-infected patients to reduce the risk of antibiotic resistance. An analysis in May revealed that of around 2,000. 72% of coronavirus patients treated in hospitals around the world. received antibiotics, although only 8 percent. developed a bacterial or fungal infection.
As bacteria become more resistant to antibiotics, the risk of catastrophic consequences increases. For example, the E. coli bacteria cause millions of urinary tract infections each year. “If an antibiotic resistant strain were to develop, the infection could spread and kill many young women,” said Lance’s Price, founder and director of the George Washington University Antibiotic Resistance Action Center.
“They would see a doctor for what they thought was a normal bladder infection and would eventually die from the blood infection because the doctors tried and failed to cure the infection, which would spread from the bladder to the kidneys and into the stream. blood, “he said.
According to Price, the coronavirus pandemic has demonstrated the “dysfunctional” nature of our public health system, which has “become the target of slow-growing, antibiotic-resistant bacteria.”
“The United States is not prepared to deal with bacterial pandemics, as evidenced by our inability to deal with many of the multi-drug resistant bacterial epidemics and pandemics recorded simultaneously,” he said.
According to Fortune, over time, bacteria become resistant to new antibiotics, so they must be used with extreme caution, and new antibiotics also need to be developed.
However, a new class of antibiotics has not been developed for decades. The companies that created them, such as Achaogen and Aradigm, have ceased operations in recent years. And pharmaceutical giants like Novartis and Allergan don’t even take it.
According to Fortune, the development of new antibiotics is not as profitable for drug manufacturers as it is for other drugs. Many drug companies have tried to develop a new antibiotic and failed, so they are spending more money developing drugs that people would take regularly rather than just when they develop an infection.
Also, companies cannot make as much money from antibiotics as from other drugs. Finally, the shelf life of antibiotics is short. Therefore, to develop new antibiotics, it is necessary to find ways to make their development a priority for pharmaceutical companies.
The UK is already receiving incentives. The country’s government is investing 60 million. Dollars for the development of antibiotics through the Innovation Fund. And the country’s National Health Service, the NHS, has established a special funding mechanism to encourage pharmaceutical companies to develop new antibiotics. Under this plan, the NHS will pay companies upfront for access to antibiotics, not for the number of pills they make.
More viruses … to fight bacteria
In addition to newer antibiotics, certain types of viruses can help fight antibiotic-resistant bacteria. There are certain types of viruses called phages that naturally kill certain bacteria. If a specific phage can be identified that kills the bacteria that has infected the person, that virus can be used to treat the infection.
Mr. Strathdee himself has personally come across this method of treatment. Her husband was infected with a superbug in 2015 that could not be destroyed by any antibiotics. As a result, he came into contact with people who analyzed phages and superbugs. In a cattle manure and sewer system where there are many phages, the researchers found a specific phage that could have killed that particular bacteria. When a cocktail of billions of such phages was injected into S. Strathdee’s husband, he made a full recovery.
“Even just me, an infectious disease epidemiologist, but my whole family’s life has been turned upside down and will never be the same again due to superbugs. And if such bacteria unexpectedly catch me, it can catch anything, because an ordinary person does not know what the size of the problem is, ”he said.
S. Strathdee is one of the founders of the IPATH Center and is currently preparing to launch the first clinical trials of phage therapy. “We need a huge library of phages to be open source to help identify phages with specific bacterial infections, so that the phages can be used in conjunction with antibiotics to kill these superbugs,” said the expert.
Frieden noted that international cooperation was needed to address this issue.
“The point is that a multifaceted response is needed. This means constant funding for US government health organizations, including the Centers for Disease Control and Prevention. This means serious support for WHO, including funding and a mandate, which means a stronger and better approach to identifying and closing the gaps in our global preparedness. “
It is strictly forbidden to use the information published by DELFI on other websites, in the media or elsewhere, or to distribute our material in any way without consent, and if consent has been obtained, it is necessary to cite DELFI as the source.
[ad_2]