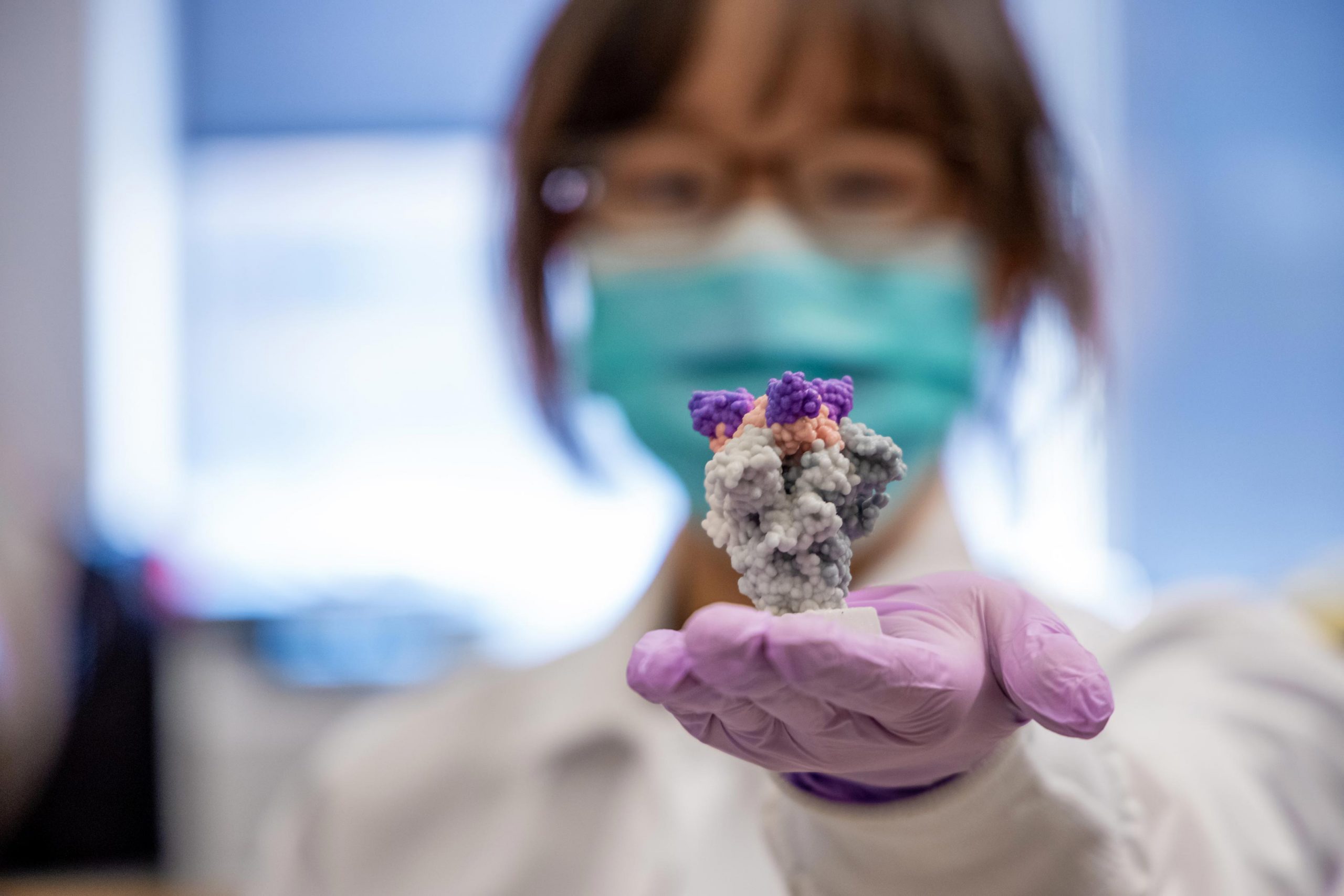

Lead author Yufei Xiang has a 3D printed model of nanobodies (purple) on top of the SARS-Co-2 spike protein (gray). Credit: UPMC
Researchers from the University of Pittsburgh School of Medicine describe in the journal ScienceNew method of small but extremely powerful ka ract dish SARS-CoV-2 Antibody fragments of saliva, which form in inhable therapeutics with the potential to prevent and treat COVID-19.
These special lama antibodies, called “nanobodies”, are much smaller than human antibodies and are often effective in neutralizing the SARS-CoV-2 virus. They’re even more stable.
“Nature is our best inventor,” said Yi Shi, PhD, senior author, assistant professor of cell biology at Pitt. “The technology we’ve developed is neutralizing nanobodies on an unprecedented basis, the Sars-Covey-2, which has allowed us to quickly discover thousands of nanobodies with unparalleled affection and uniqueness.”
To make these nanobodies, Shi turned to a black red named Shi Li – looks like so and so he shares his moniker with Sheena’s black Labrador.
Science. Yi Shi, senior author of a paper published in Science, explains how “nanobodies” can become a powerful new weapon against the COVD-19 epidemic. Credit: UPMC
Shi and colleagues vaccinated Lalama with a piece of SARS-COV-2 spike protein and about two months later, the animal’s immune system produced mature nanobodies against the virus.
Using a mass spectrometry-based technique that has been perfecting Shi for the past three years, Shife Lab’s research assistant lead author Yufei Xiang identified nanobodies in the parent’s blood that are linked to SARS-Co-2.
Then, with the help of the Pitts Center for Vaccine Research (CVR), the scientists exposed their nanobodies to the SARS-Cavi-2 virus to survive and found that just one fraction of the nanogram could neutralize the virus enough to protect one million cells from infection. Is.

Valley Lalama. Credit: Sonia Paske, Caprelox Ltd.
These nanobodies represent some of the most effective therapeutic antibody candidates for SARS-CV-2, hundreds to thousands of times more effective than other llama nanobodies discovered by similar phage display methods used for decades to detect fish for human monoclonal antibodies.
Shiny nanobodies can sit at room temperature for up to six weeks and can come in the form of incredible mist to deliver antiviral therapy directly to the lungs where they are most needed. Since SARS-CoV-2 is a respiratory virus, nanobodies can detect it in the respiratory tract before it has a chance to harm it.
In contrast, conventional SARS-Co-2 antibodies require IV, which dilutes the product throughout the body, costing the patient and insurers around $ 100,000 per course of treatment.
“Nanobodies can potentially cost very little,” Shea said. “They are ideal for considering the urgency and severity of the current crisis.”
Cheng Zhang, Ph.D., and Dina Snydman-Duhovni, Ph.D., at Pete at the Hebrew University of Jerusalem. Together, the team found that their nanobodies used a variety of methods to block SARS-Co-2. Infection. This ripens nanobodies for bioengineering. For example, nanobodies that bind to different regions on the SARS-Covi-2 virus, like a Swiss Army knife, change part of the virus and become drug-resistant, can bind together.
“As a virologist, it is incredible to see how the ingenuity of the Lama antibody pay generation can be translated into the formation of powerful nanoparticles against the clinical isolates of SARS-Cavi-2,” said Paul L. Dupree, co-author of the study and director of CVR. .
Reference: “Versatile and multivalent nanobodies effectively thwart SARS-CoV-2” Yufe Xiang, Sham Nambuli, Zhengyun Xiao, Hang Liu, Ze Sang, W. Paul Duprex, Dina Snydman-Duhovni, Cheng Zhang and Yi Shi, November 5, 2020 Science.
DOI: 10.1126 / Science.B.44747
Additional authors on the study include Sham Nambuli, Ph.D., Zhengyun Xiao, Hang Liu, Ph.D., and Ze Sang, all of Pete.
Funding for the study is provided by the National Institutes of Health (R35GM137905 and R35GM128641), the University of Pittsburgh Institute of Clinical and Translational Sciences, the Peat Center for Vaccine Research, and the DSF Charitable Foundation.