
Ted Horowitz | Getty Images
One of the surprising aspects of the human response to the Kovid-1p epidemic is that scientists quickly developed studies of every aspect of the virus to reduce the loss of life and plan to return to normal. At the same time, a non-coronavirus research ground at a nearby location.
Research laboratories and office fees are closed to all but workers, many scientists are stuck at home, their field work and meetings are canceled and planned experiments are kicking off the road as they struggle to figure out how to continue their research programs. Is. Many jumped at the chance to write grants and papers; Some – in the midst of caring for children – came up with a strategic workaround to keep the scientific interest flowing.
To find out how researchers from different fields are managing, Knowledgeable Magazine Scientists spoke with an array of scientists and technicians – experts in keeping the vital vital strains of fruit flies alive, clinicians working to keep telescopes safe during lectures, and the maintenance chief of an astronomer observatory working on standby, and a pediatrician. . Rare genetic disease. Here are some snippets of scientific life during an epidemic.
Agnieszka Chekoviz, Stanford University School of Medicine

Pediatrician Agnieszka Chekoviz, Stanford University[/ars_img]Chekowis is a pediatrician in Stackford’s Department of Stem Cell Transplantation and Regenerative Medicine, where he leads a research group that develops new therapies and conducts clinical trials on rare genetic diseases.
Agnieszka Chekoviz’s father suffers from severe Parkinson’s disease. Coronavirus epidemics forced him to stay indoors and away from people, robbing him of the physical condition and social interaction he needed to cope with his disease. Leaving him in the hospital since the recent fall, brought additional concern that he could contract Kovid-19 there and make him more isolated. >> For Checoviz, the challenges that coronavirus has posed to those who run medical tests on his condition are quickly relieved. Including those she runs, including patients in hospitals across the country. “Am I traveling to a clinical site right now for a new Parkinson’s treatment?” She said. “Not sure.”
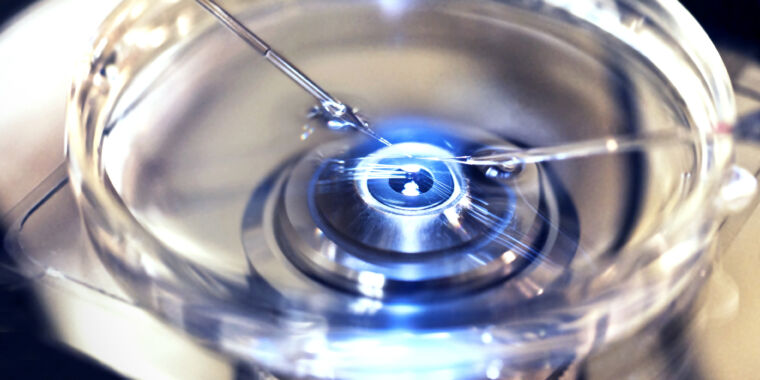
The epidemic forced the Czechoslovakia to stop a clinical trial to monitor for a rare genetic disease in children called fungal anemia, a condition that impairs the body’s ability to repair damaged DNA and lead to bone marrow failure and cancer. The treatment that Czech Koviz and his colleagues are investigating involves inserting a healthy copy of a missing or defective gene into a stem cell that makes blood from a patient’s bone marrow and then re-inserting those cells into the patient.
“Every aspect of everything I do is greatly affected by the epidemic,” Chekowis says. A clinical trial in its early stages involves testing the safety of the treatment. But during the initial shutdown – which began in mid-March and lasted for two months, his patients could not easily travel to Stanford for the necessary follow-up visits, and remote monitoring was difficult.
“There are special blood tests and bone marrow tests that we need to do. In particular, it is important to get samples to make sure patients, for example, are not developing leukemia, “he says.” There is no way to know without examining the bone marrow. “Overcoming major obstacles to evaluating his patients. Fell.
Other early-stage trials designed to determine the effectiveness of treatment also had to stop enrolling new patients. Because speed is important when it comes to treating fungal infections – children probably lose stem cells all the time – any delay in treatment can be a big concern for their parents. Chekowicz had to explain to him why the trial was temporarily suspended. “It was really challenging to have these discussions with those families,” he says.
As travel and workplace restrictions eased, families began traveling to Stanford in June, but many families are hesitant again as the infection grows, Chekowies says. Fortunately, her trial is short, so she can guide each family through the process of safely resuming tests and continuing follow-up. Even his own team has to follow strict safety protocols. For example, even though it has 10 members in its lab, there can be only two in the lab at any one time, and only one parent is allowed in the clinic with the child.
Not all clinical trials can focus as much on individual patients. A large trial with hundreds of patients may involve multiple sites and require more monitoring, so it remains difficult to resume. Also, restrictions on working on full bore are slowing the pipeline for new therapies. “The effect, we won’t see for many years to come,” Chekowis says.
Abolhasan Zawahiri, University of Maryland, College Park

Jawahari is a particle physicist and a member of the LHCB, one of the main experiments at the Large Hadron Collider (LHC) at the Particle Physics Laboratory CERN near Geneva.
In December 2018, before the coronavirus epidemic began, the LHC closed for updates. Placed in a 27-kilometer-long tunnel about 100 meters underground, the LHC has propelled two beams of protons, one clockwise and one counterclockwise, making them collide in four places. There, discovering evidence of new physics, Atlas, CMS, LHCB and Ellis-four giant subterranean detectors are explored from the debris created by the collision. (For example, Atlas and CMS found the Higgs boson, the basic particle of the Higgs field, which gives all the initial particles their mass.) , LHC needed to increase the intensity of its proton beam. As a result, four detectors also needed to be upgraded, resulting in higher temperature control and increased radiation at the point of collision of the particles. The epidemic was set to resume around May 2021 until scientists’ precautionary plans were lifted.
LHC and its four detectors are each operated by a separate collaboration. CARN, which manages LHC, hopes to resume the collision by February 2022. “They think they can go to the accelerator if no major catastrophic events happen.” But the effect on the four detectors is less clear.
For the LHCB upgrade, Jawahri’s team at the University of Maryland was working to build nearly 1,000,000 highly sensitive electronic circuit boards. These boards have to be “burned” before they can be sent to CERN. “We put them in the oven, literally cook the boards and then run detailed tests to prepare them so we can put them in the accelerator and run for 10 to 20 years,” says Jawahari. “And none of that happened during the epidemic.”
The team resumed its work in June, but restrictions were placed by the state of Maryland. Jawahari runs two labs, and for months only two people were allowed in one experiment at a time and three in another, making progress very slow. Still, his team is fortunate that it is not dependent on the supply of countries hit hardest by the coronavirus. Other labs weren’t so lucky. Scientists in Milan, for example, built some electronics and detector components for the LHCB, and sensors from a lab at Syracuse University in New York relied on shipments to Milan. When the height of the Milan epidemic was completely shut down, Syracuse also stopped working on Milan-based dependent components.
The lockdown for the jeweler had a silver lining. The most recent part of the LHC produced about 25 gigabytes of data per second – but its team had little time to do any analysis before the epidemic. “We were complaining that we were spending all our time creating new tools and the data kept coming,” he says. When he and his team were kicked out of their labs, they turned to their data backlog. “We can do real physics,” he says. “We are preparing to publish some papers.”