[ad_1]
A large study led by the World Health Organization suggests that the antiviral drug remdesivir did not help hospitalized patients with COVID-19, in contrast to an earlier study that made the drug a standard of care in the United States and many others. countries.
The results announced Friday do not negate the earlier ones, and the WHO study was not as rigorous as the previous one led by the U.S. National Institutes of Health. But concerns are mounting about how much value the expensive drug places because neither of the Studies have found that it can improve survival.
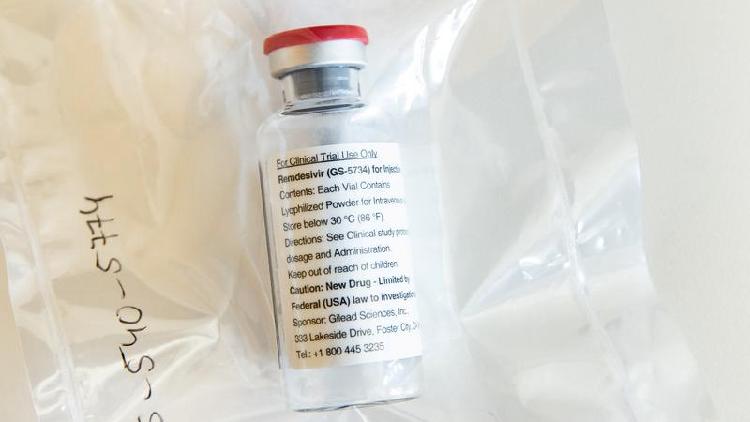
The drug has not been approved for COVID-19 in the US, but was authorized for emergency use after the previous study found it shortened recovery time by five days on average. It is approved for use against COVID-19 in the UK and Europe, and is among the treatments that US President Donald Trump received when he became infected earlier this month.
The WHO study involved more than 11,000 patients in 30 countries. About 2,750 were randomized to obtain remdesivir. The rest received the antimalarial drug hydroxychloroquine, immune-boosting interferon, the antiviral combination lopinavir-ritonavir, or just usual care. The other drugs have been largely ruled out for COVID-19 by previous studies, but not remdesivir.
Rates of death after 28 days, need for ventilators, and time in hospital were relatively similar for those who received remdesivir versus usual care.
The results have not been published in a journal or reviewed by independent scientists, but instead were published on a site that researchers use to share results quickly.
Results row
“The big story is the finding that remdesivir does not have a significant impact on survival,” Martin Landray, a professor at the University of Oxford who led other research on the treatment of coronavirus, said in a statement.
“This is a drug that needs to be given by intravenous infusion for five to 10 days” and costs about $ 2,550 per course of treatment, he said. “COVID affects millions of people and their families around the world. We need scalable, affordable and equitable treatments.”
WHO spokeswoman Dr. Margaret Harris attributed the difference in the conclusions of the two studies to the fact that the WHO was larger. “It’s just a much higher powered study,” he said, adding that “it’s four times the number of people in all the other studies.”
However, Dr. Andre Kalil, an infectious disease specialist at the University of Nebraska who helped lead the remdesivir study in the US, said that the WHO study was poorly designed, making his conclusions sound. less reliable. Patients and doctors knew what treatment they were using, there was no placebo infusion to help avoid biased reports of risks or benefits, there was little information about the severity of patients’ symptoms when the treatments started, and much missing data, he said. .
“Poor quality study design cannot be fixed with a large sample size, no matter how large,” Kalil wrote in an email.
Additionally, the WHO study evaluated 10 days of remdesivir, so some patients may have been hospitalized longer than necessary to complete treatment, making their length of stay look poor compared to others receiving the remdesivir. usual care.
Remdesivir’s maker, Gilead Sciences, said in a statement that the results are inconsistent with more rigorous studies and have not been fully reviewed or published.
Richard Peto, an independent statistician hired by the WHO to analyze the results of its Solidarity trial, dismissed Gilead’s criticism.
“It’s a reliable result, don’t let anyone tell you otherwise, because they will try,” Peto told reporters. “This is real world evidence.”
(Cover: A Gilead Sciences COVID-19 antiviral remdesivir ampoule is displayed during a press conference at Eppendorf University Hospital (UKE) in Hamburg, Germany, April 8, 2020./Reuters)