
[ad_1]
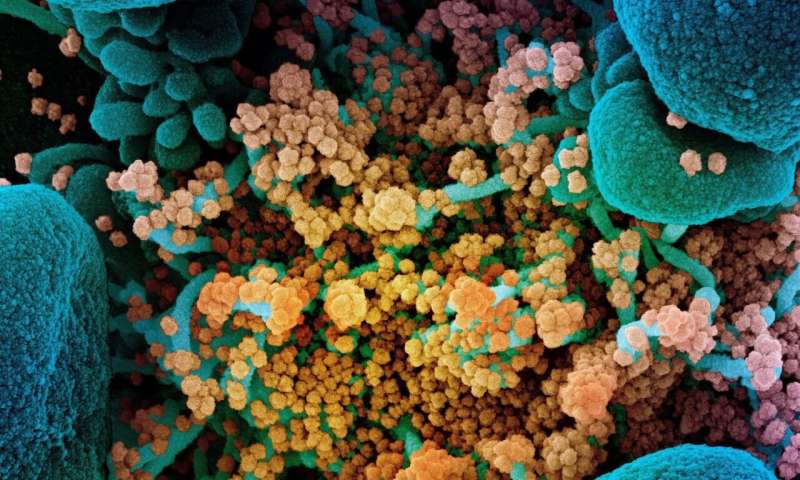
Colored scanning electron micrograph of a dying cell (blue) heavily infected with SARS-CoV-2 (yellow), the virus that causes COVID-19. Credit: NIAID Integrated Research Facility, Fort Detrick, Maryland.
A tool designed to detect viral history in a drop of blood has been improved in the era of COVID-19. VirScan, a technology that can determine which of more than 1,000 different viruses has infected a person, can now also detect evidence of coronavirus infection, including SARS-CoV-2. In an article published in Sciences, researchers from Brigham and Women’s Hospital and Harvard Medical School offer a treasure trove of details about the antibody response to SARS-CoV-2 and how this response may differ in people who later have a more severe case of COVID-19 .
“This may be the most in-depth serological analysis of any virus in terms of resolution,” said corresponding author Stephen Elledge, Ph.D., Gregor Mendel professor of genetics at Brigham and HMS. “Now we understand much, much more about the antibodies generated in response to SARS-CoV-2 and how often they are produced. The next question is, what do those antibodies do? We need to identify which antibodies have an inhibitory capacity or which ones, if they do. there is, it can promote the virus and help it get into immune cells. “
In their analysis, Elledge and his colleagues closely examined antibody responses to SARS CoV-2 by using VirScan to analyze blood samples from 232 COVID-19 patients and 190 pre-COVID-19 controls. The team identified 800 sites on the virus that the immune system can recognize, known as epitopes. Not all epitopes are the same; some can be recognized by neutralizing antibodies, which can elicit a response that clears the infection. However, if the body creates antibodies against other epitopes, it can launch a less effective response, giving the virus an advantage. In some cases, including the related coronavirus that causes SARS, viruses can even benefit from the body’s antibody response, using antibodies to enter cells in a phenomenon known as antibody-dependent enhancement.
In the case of SARS-CoV-2, the team detected a range of frequencies of antibodies against various epitopes. Many were public epitopes, regions recognized by the immune systems of large numbers of patients. A public epitope was recognized by 79 percent of COVID-19 patients. Others are considered private and recognized by only a few or even an individual. Ten epitopes were found in regions essential for viral entry and are probably recognized by neutralizing antibodies. The team used the most discriminating epitopes to develop a rapid diagnostic test.
The team’s epitope findings may have important implications for vaccines. If the immune system’s response to public epitopes is not protective, or even does not give the virus an advantage, vaccines will need to target other regions of the virus to stimulate the immune system.
Additionally, the team found that there are several conserved epitopes in coronaviruses and that the immune system is likely to try to reuse antibodies against them when infected with SARS-CoV-2, a possible explanation for why so many serological tests for COVID-19 produce false positives.
The team further analyzed where and when the different antibody responses occurred, and found that severe COVID-19 patients were more likely to launch a stronger and broader response against SARS-CoV-2, possibly because their initial immune response did not. managed to control the infection early. Among hospitalized patients, men produced more antibodies than women. The researchers also compared the viral histories of hospitalized and non-hospitalized COVID-19 patients and found that hospitalized patients were much more likely to have had CMV and HSV-1, two common herpes viruses. However, the researchers note that it is difficult to draw conclusions about causation given that the group of outpatients was younger and comprised of a higher percentage of white people and women, a demographic that generally has lower rates of infection with CMV.
Elledge envisions his studies as a stepping stone to identifying the most effective antibodies and obtaining them.
“Our article illuminates the landscape of antibody responses in COVID-19 patients,” Elledge said. “Next, we need to identify the antibodies that bind to these recurrently recognized epitopes to determine whether they are neutralizing antibodies or antibodies that could exacerbate patient outcomes. This could inform the production of improved diagnostics and vaccines for SARS-CoV- two”.
Antibody responses in COVID-19 patients could guide vaccine design
“Viral epitope profile of COVID-19 patients reveals cross-reactivity and correlates of severity.” Sciences (2020). science.sciencemag.org/cgi/doi… 1126 / science.abd4250
Provided by Brigham and Women’s Hospital
Citation: VirScan Offers New Insights into the COVID-19 Antibody Response (2020, September 29) Retrieved September 29, 2020 from https://medicalxpress.com/news/2020-09-virscan-insights-covid-antibody- response.html
This document is subject to copyright. Apart from any fair dealing for private study or research purposes, no part may be reproduced without written permission. The content is provided for informational purposes only.
[ad_2]