[ad_1]
As the world grapples with the current crisis of the coronavirus pandemic, scientists warn that the infection may pose another serious threat to human health, in the form of a “silent wave” of neurological consequences that could follow from the virus.
While the specific risks remain hypothetical at this time, the concerns are very real. In fact, a similar long-term effect was seen after the Spanish flu pandemic of the last century.
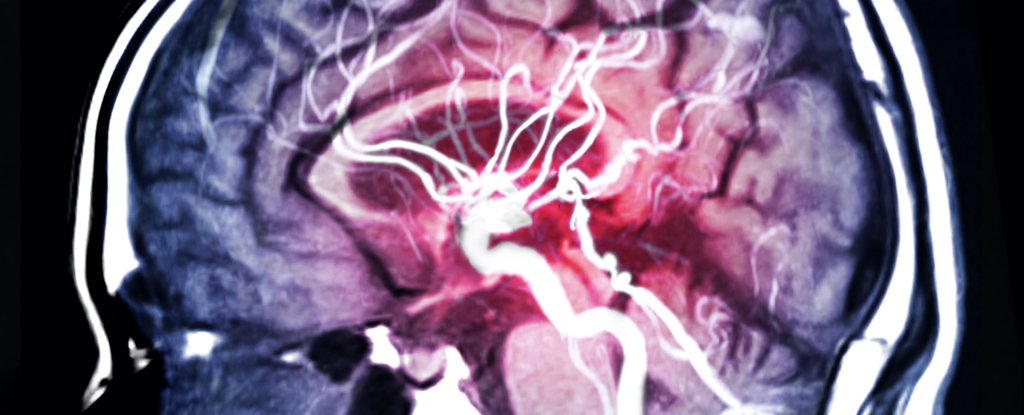
We already know that COVID-19 has links to brain damage, neurological symptoms, and memory loss. What is less clear is how the infection can cause these paralyzing symptoms, in what volume and with what final effect.
“Although scientists are still learning how the SARS-CoV-2 virus is capable of invading the brain and central nervous system, the fact that it is entering is clear,” says neuroscientist Kevin Barnham of the Florey Institute for Neuroscience and Mental Health. in Australia.
“Our best understanding is that the virus can cause damage to brain cells, with the potential for neurodegeneration from there.”
How to measure that potential is the big question.
In a new study, Barnham and his co-authors propose that the “third wave” of the COVID-19 pandemic might not be a resurgence of coronavirus infections, but a subsequent rise in virus-associated Parkinson’s disease cases, seeded by neuroinflammation, triggered in the brain as an immune response to the virus.
There is no solid evidence yet to confirm that such an increase in parkinsonism will ultimately result, it is worth noting.
But something very similar to this happened once before, during the last and most comparable pandemic to take over the world: the Spanish flu of 1918, where a pandemic-related form of brain inflammation called encephalitis lethargica increased the risk of parkinsonism by two. or three. times.
“We can understand the neurological consequences that followed the Spanish flu pandemic in 1918,” says Barnham.
“Given that the world population has been hit again by a viral pandemic, it is very worrying to consider the potential global increase in neurological diseases that could develop along the way. The world was taken by surprise the first time, but it is not.” It is not I need to come back. “
While the researchers acknowledge that there is currently insufficient data to quantify the increased risk of developing Parkinson’s disease in relation to COVID-19 infections, they suggest that the best way to identify future cases early would be through long-term detection. term of subsequent SARS-CoV-2 cases – recovery, follow-up of manifestations of neurodegenerative diseases.
The new research just so happens to coincide with the publication of a case report from Israel that highlights the kinds of risks that Barnham and his colleagues are anticipating, even if the episode itself remains far from clear.
In what appears to be the first documented case of a patient developing Parkinson’s disease after a previous SARS-CoV-2 infection, doctors relate how a 45-year-old man was hospitalized in March with symptoms of COVID-19, experiencing coughing and muscle pain. and loss of smell.
During a subsequent period of isolation in a COVID-19 facility, he began to experience difficulties communicating, both speaking and writing, and also showed signs of trembling and difficulty walking, with subsequent tests indicating a diagnosis of Parkinson’s disease. .
While the man’s doctors acknowledge that the mechanism that triggered his neurodegeneration is unclear, they say it’s hypothetically possible that his condition was somehow triggered by inflammation in the brain caused by the virus, after the infection took hold. of your central nervous system.
That said, the short window of time between their COVID-19 infection and the development of Parkinson’s symptoms makes the hypothesis unlikely, they admit, calling the temporal association “intriguing,” even if we can’t conclude much with certainty from this isolated case.
In this case, the man had no family history of Parkinson’s disease and no obvious genetic signs of predisposition, but some believe it is possible that the infection could exacerbate or accelerate the development of latent Parkinson’s that has yet to be revealed.
“The COVID-19 infection may have been a stressor that brings previously subtle and unrecognized symptoms to a point of consciousness,” University of Cincinnati neurologist Alberto Espay, who was not involved in the study, told MedPage Today. the case.
“It’s not that those exposures caused Parkinson’s disease, but rather that they acted as precipitants, exacerbating the subtle symptoms of Parkinson’s disease to a threshold of severity that makes them first noticeable to patients and clinicians.”
While that’s largely speculative, at least for now, it does emphasize the possibility that future cases of Parkinson’s after COVID-19 could be caught early, if we only know what to look for and recognize them before the condition has developed. completely. at which point mitigation is no longer an option.
“By waiting until this stage of Parkinson’s disease to diagnose and treat, you’ve already lost the window for neuroprotective therapies to have the desired effect,” says Barnham.
“Along with a strategic public health approach, tools for early diagnosis and better treatments will be key.”
Findings are reported in the Parkinson’s Disease Journal.