
[ad_1]
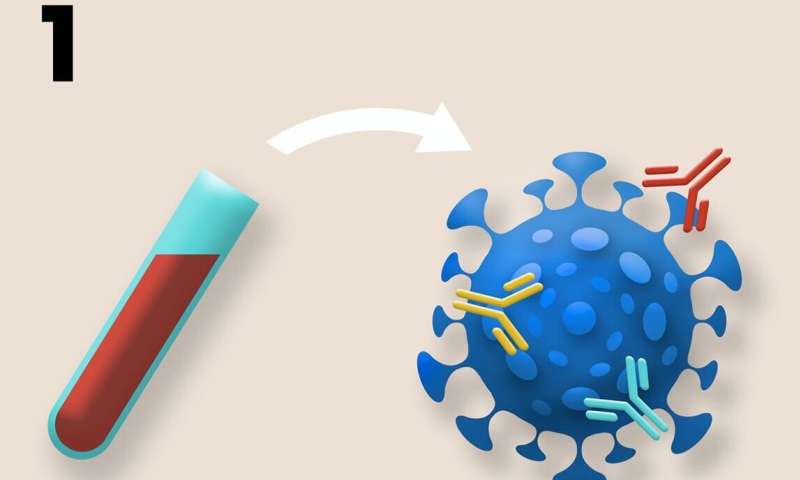 Schematic illustrating three ways that standard samples from COVID-19 clinical trials can be reused to assess the risk of evolving vaccine resistance. 1. The complexity of B and T cell responses can be measured using blood samples. The different neutralizing antibodies are represented above in different colors. More complex responses indicate evolutionarily more robust immunity. 2. The effect of vaccination on the potential for transmission can be assessed by collecting viral titer data using routine nasal swabs. Plaque assays from multiple vaccinated and control individuals are compiled into a histogram. Undetectable viral titers suggest little or no potential for transmission, due to complete immune protection or no exposure. High viral titers suggest a high transmission potential due to the absence of a protective immune response. Intermediate viral titers, marked above with an asterisk, suggest a moderate transmission potential due to partial protection of the vaccine. Intermediate titers indicate a higher risk of resistance evolution, since a diversity of pathogens can be generated within hosts and selection can act during transmission between hosts. 3. Pre-existing variation in vaccine resistance can be assessed by retrieving genome sequences from nasopharyngeal swabs from symptomatic COVID-19 cases included in the study. In a double-blind, placebo-controlled study, any significant difference in the genome sequences of samples from vaccinated and control individuals would suggest at least partial resistance to the vaccine. Credit: Kennedy et al, 2020 (PLOS Biology, CC BY 4.0)
Schematic illustrating three ways that standard samples from COVID-19 clinical trials can be reused to assess the risk of evolving vaccine resistance. 1. The complexity of B and T cell responses can be measured using blood samples. The different neutralizing antibodies are represented above in different colors. More complex responses indicate evolutionarily more robust immunity. 2. The effect of vaccination on the potential for transmission can be assessed by collecting viral titer data using routine nasal swabs. Plaque assays from multiple vaccinated and control individuals are compiled into a histogram. Undetectable viral titers suggest little or no potential for transmission, due to complete immune protection or no exposure. High viral titers suggest a high transmission potential due to the absence of a protective immune response. Intermediate viral titers, marked above with an asterisk, suggest a moderate transmission potential due to partial protection of the vaccine. Intermediate titers indicate a higher risk of resistance evolution, since a diversity of pathogens can be generated within hosts and selection can act during transmission between hosts. 3. Pre-existing variation in vaccine resistance can be assessed by retrieving genome sequences from nasopharyngeal swabs from symptomatic COVID-19 cases included in the study. In a double-blind, placebo-controlled study, any significant difference in the genome sequences of samples from vaccinated and control individuals would suggest at least partial resistance to the vaccine. Credit: Kennedy et al, 2020 (PLOS Biology, CC BY 4.0)Like bacteria that develop resistance to antibiotics, viruses can develop resistance to vaccines, and the evolution of SARS-CoV-2 could undermine the effectiveness of vaccines currently in development, according to an article published on 9 November in the open access journal. PLOS Biology by David Kennedy and Andrew Read from Pennsylvania State University, USA The authors also provide recommendations to vaccine developers to minimize the likelihood of this outcome.
“A COVID-19 vaccine is urgently needed to save lives and help society return to its normal pre-pandemic state,” said David Kennedy, assistant professor of biology. “As we have seen with other diseases, such as pneumonia, the evolution of resistance can quickly render vaccines ineffective. By learning from these previous challenges and implementing this knowledge during vaccine design, we can maximize the long-term impact. Vaccines for COVID-19. “
The researchers specifically suggest that standard blood samples and nasal swabs taken during clinical trials to quantify individuals’ responses to vaccination can also be used to assess the likelihood that the vaccines being tested will drive the evolution of resistance. For example, the team proposes that blood samples can be used to assess the redundancy of immune protection generated by candidate vaccines by measuring the types and amounts of antibodies and T cells present.
“Just as antibiotic combination therapy slows the evolution of antibiotic resistance, vaccines that are designed to induce a redundant immune response, or one in which the immune system is encouraged to target multiple sites, called epitopes , on the surface of the virus, evolution of vaccine resistance, “said Andrew Read, Evan Pugh Professor of Biology and Entomology and director of the Huck Institutes of Life Sciences. “That’s because the virus would have to acquire multiple mutations, rather than just one, to survive attack by the host’s immune system.”
The researchers also recommend that nasal swabs typically collected during clinical trials can be used to determine viral titer or the amount of virus present, which can be considered an indicator of the potential for transmission. They noted that strongly suppressing virus transmission through vaccinated hosts is key to slowing the evolution of resistance, as it minimizes the opportunities for mutations to arise and reduces the opportunities for natural selection to act on the mutations that arise.
In addition, the team suggests that genetic data acquired through nasal swabs can be used to examine whether a vaccine-driven selection has occurred. For example, differences in alleles, or forms of genes that arise from mutations, between viral genomes collected from vaccinated versus unvaccinated individuals would indicate that selection has taken place.
“According to the World Health Organization, at least 198 COVID-19 vaccines are under development, and 44 are currently under clinical evaluation,” Kennedy said. “We suggest that the risk of resistance be used to prioritize investment among equally promising candidate vaccines.”
Follow the latest news on the coronavirus outbreak (COVID-19)
PLOS Biology (2020). DOI: 10.1371 / journal.pbio.3001000
Provided by Pennsylvania State University
Citation: Could SARS-CoV-2 Develop Resistance to COVID-19 Vaccines? (2020, November 9) Retrieved on November 9, 2020 from https://medicalxpress.com/news/2020-11-sars-cov-evolve-resistance-covid-vaccines.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no part may be reproduced without written permission. The content is provided for informational purposes only.
[ad_2]