
[ad_1]

The file photo shows a measles, mumps and rubella vaccine on the counter of a pediatric clinic. “It is completely unacceptable that children continue to die from measles in 2019,” said the President and CEO of the Philippine Red Cross.
Image Credit: AP
Dubai: It has been a puzzling fact since the coronavirus pandemic began: Most children seem to avoid severe cases of COVID-19. New research offers a possible explanation, and it comes down to vaccination against mumps. A peer-reviewed study recently published in the journal mBio (the open access journal of the American Society for Microbiology) found a “statistically significant inverse correlation” between mumps “titer” levels and COVID-19 severity.
A titer is a laboratory test that measures the presence and amount of antibodies in the blood, indicating immunity to disease. Since March 2020, it has been theorized that the MMR vaccine provides protection against severe COVID by reducing the inflammation associated with SARS-CoV-2. But so far, there is no scientific evidence to prove it. The study looked at MMR markers among recovered (convalescent) COVID-19 patients, whose infection was previously confirmed by PCR testing.
80 people studied
The research team divided the 80 convalescent from COVID-19 into two groups: the first consists of 50 subjects who would mainly have MMR antibodies from the MMR II vaccine. The second group includes 30 subjects who would have primarily MMR antibodies from sources other than the MMR II vaccine, including previous measles, mumps, and / or rubella illnesses. Both the titer and the severity levels were measured according to standardized scales. What they found was surprising: People with the highest mumps antibody titers had asymptomatic COVID-19.
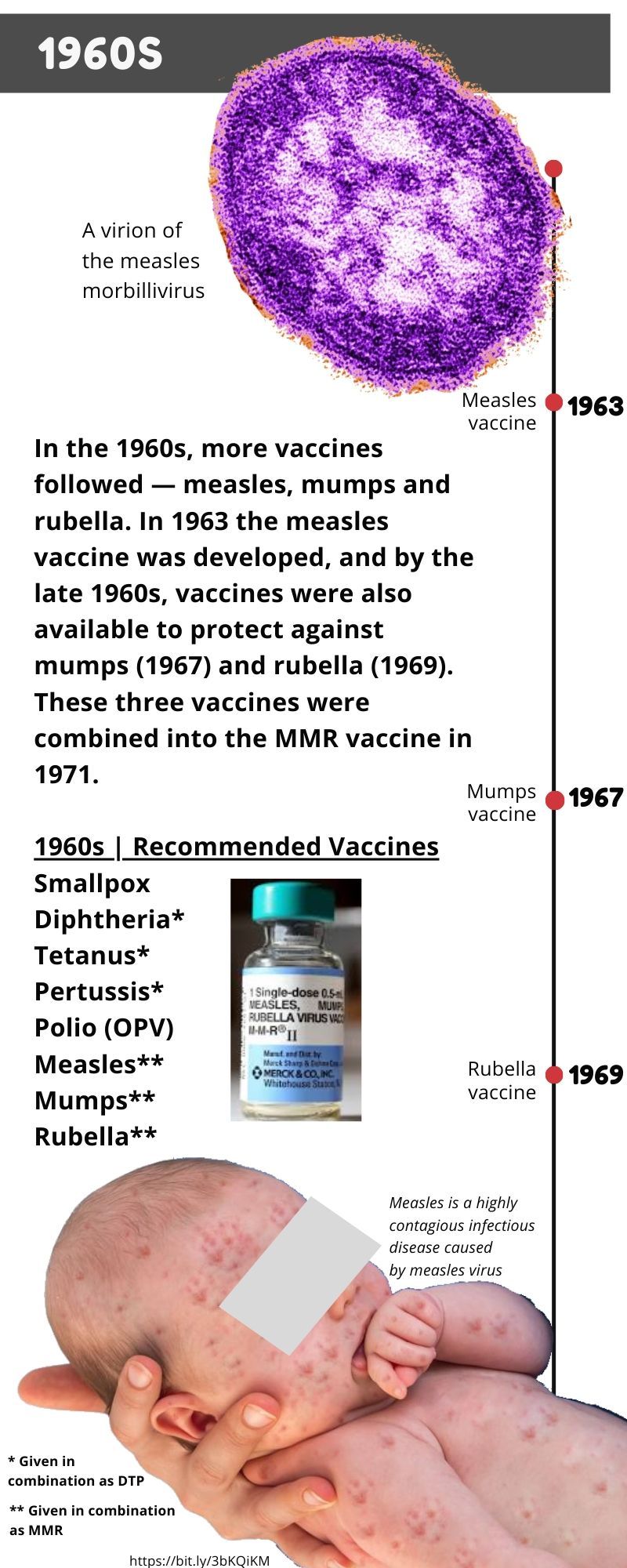
Image Credit: Gulf News
Inverse correlation
The researchers stated in the November / December 2020 issue of the journal that among 50 COVID-19 patients under the age of 42 who had received MMR II as children, the higher were their titers or levels of so-called “IgG antibodies.” produced by the vaccine and directed against the mumps virus in particular, the less severe its symptoms are.
Within the MMR II group, mumps titers of 134 to 300 arbitrary units (AU) / ml (n = 8) were found only in those who were functionally immune or asymptomatic. Those with mild symptoms had mumps titers below 134 AU / ml (n = 17). Those with moderate symptoms had mumps titers below 75 AU / ml (n = 11). All those who had been hospitalized and required oxygen had mumps titers below 32 AU / ml (n 5). “Our results demonstrate that there is a significant inverse correlation between MMR II mumps titers and COVID-19 severity,” the team stated.
Children: lower death rate and COVID cases
The sample of 80 convalescents is relatively small and the researchers stated that it must be expanded to validate their results. Still, the new findings “may explain why children have a much lower COVID-19 case rate than adults, as well as a much lower death rate,” said co-author Jeffrey Gold, chairman, in a statement. of the World Organization, in Watkinsville, Georgia. . “Most children get their first MMR vaccine around 12 to 15 months of age and a second between 4 and 6 years of age.”
BAT MUMPS Virus
In 2012, the US National Institutes of Health reported that a bat virus highly similar to the mumps virus was completely sequenced from the spleen of a bat. Mumps virus belongs to the large family of viruses ‘Paramyxoviridae’ which includes some of the most important human and livestock viruses, such as measles, distemper, mumps, parainfluenza, Newcastle disease, respiratory syncytial virus and metapneumoviruses.
What is an antibody titer?
An antibody titer is a type of blood test that determines the presence and level (titer) of antibodies in the blood. This test is done to find out if there is an immune reaction caused by foreign invaders (antigens) in the body. To determine a titer level, a blood sample is taken and tested. If the test is positive (above a particular known value), it shows that the individual has immunity.
In March 2020, Jeffrey Gold, the lead researcher, presented the theory after noting that recent large-scale MMR vaccination campaigns were associated with the countries with the fewest deaths from COVID-19. Another Cambridge study also made the same observation and looked at protein “homology” (similarity due to shared ancestry) between the COVID-19 virus and the rubella virus.
Homology
In biology, homology is the similarity due to shared ancestry between a pair of structures or genes in different taxa (groups or populations of an organism or organisms that taxonomists consider to form a unit).
Induce antibodies
Vaccines induce a variety of different antibodies to protect against a virus, since each part of an antigen stimulates different antibodies. Titer tests determine seropositivity (presence or levels in blood) based on a reduced set of antibody concentrations. However, they do not measure the viral neutralizing power of all the different antibodies related to a virus. It means that a titer test does not specifically indicate which of the many antibodies present in the blood is responsible for killing a specific virus.
Since March 2020, scientists led by Gold had already hypothesized that MMR II could be cross-protective against COVID-19. However, it has been thought that there is only a small subset of antibodies related to measles, mumps, or rubella that can protect against COVID-19. The researchers said they had considered the various ways that individuals develop antibodies related to MMR. To determine differences in the effect on titer values, the researchers looked at differences in age groups and the year in which various versions of the vaccines were introduced.
For example, they cited that older adults, including virtually everyone born before 1957, likely have MMR antibodies from naturally acquired infections. Meanwhile, individuals may have developed antibodies to Merck’s current MMR II vaccine (initially licensed in 1979), which includes the Edmonston strain of measles, the Jeryl Lynn mumps strain (level B), and the Wistar RA 27/3 strain. rubella.
The team also claimed that people who may have developed antibodies from “monovalent” vaccines (an injection, a targeted virus) against measles, mumps or rubella. Still, people may have antibodies to other combination vaccines, including Merck’s original MMR vaccine, which uses the less effective HPV-77 DE-5 strain of rubella.
Bat rubella virus
Rubella was first described in 1814. The origins of the disease and its causative agent, the rubella virus (Matonaviridae: Rubivirus), remain unclear. Ruhugu virus, the closest relative of the rubella virus, was found in apparently healthy cyclops leaf-nosed bats (Hipposideros cyclops) in Uganda.