
[ad_1]
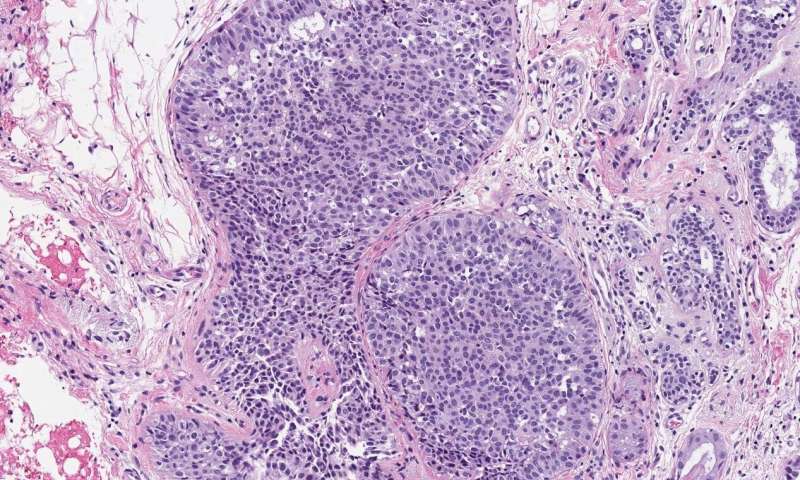
A microscopic image of breast tissue showing proliferative benign breast disease, including abnormal cells. Credit: Hospital del Mar Medical Research Institute, Barcelona, Spain
Benign breast diseases (BBD), which are non-cancerous disorders of the breast, such as lumps, are known to increase the chances of later breast cancer. Now, a team of Spanish researchers has found that the way BBD is detected as part of a national screening program is an indication of which ones are more likely to become cancerous.
The findings of a team led by Professor Xavier Castells, head of the epidemiology department of the Institute of Medical Research at Hospital del Mar, Barcelona, Spain, will be presented at the XII European Breast Cancer Conference on Saturday.
BBD detected the first time a woman undergoes a breast screening (usually at age 50 in Spain and many other European countries with national screening programs) is classified as “prevalent” BBD, while those detected in subsequent visits, which They occur every two years in Spain, they are classified as “incident” BBD.
Dr. Marta Román, senior researcher in the epidemiology department of the Hospital del Mar Medical Research Institute, said at the conference: “Our results show that women with a benign breast disease diagnosed from the second screening have a significantly subsequent risk greater than those with a BBD diagnosed in their first mammographic exam “.
The researchers analyzed data from 629,087 women who underwent 2,327,384 screening mammograms between 1995 and 2015, and followed them through 2017. They found that women diagnosed with incident BBD were 2.67 times more likely to develop breast cancer than women without BBD, while women with prevalent BBD had a 1.87 times higher risk.
They also classified BBDs as non-proliferative or proliferative, depending on whether or not the breast tissue showed an increase in the growth of certain cells, such as ductal cells found in ductal hyperplasia in which there is an overgrowth of overlying cells. the ducts. inside the chest.
They found that women with proliferative BBD were 3.28 times more likely to develop breast cancer compared to women without breast disease, while women with non-proliferative BBD had a 1.96 times greater risk.
Dr. Roman said: “We found the highest risk of breast cancer in women with incident proliferative BBD. They had an almost four times higher risk of breast cancer compared to women without BBD.”
Women with an incident nonproliferative BBD were 2.39 times more likely to develop breast cancer later compared to women without BBD; women with proliferative and prevalent BBD had a 2.85 times higher risk; and women with prevalent nonproliferative BBD had a 1.63 times higher risk.
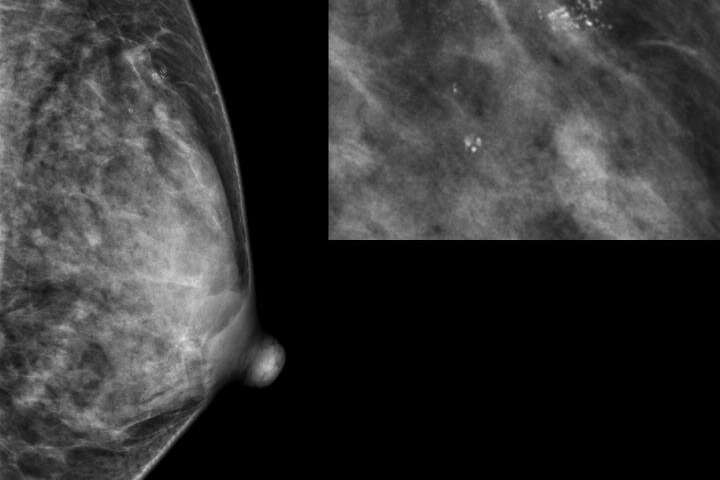
Radiological image of a suspicious finding. A biopsy would be needed to clarify if it is a benign breast disease and if more investigations are needed. Credit: Hospital del Mar Medical Research Institute, Barcelona, Spain
The researchers hope their findings will be useful in designing personalized breast cancer detection strategies to improve the effectiveness of breast cancer detection.
“How likely a woman will benefit from screening mammography depends on her risk of developing clinically significant breast cancer in her lifetime,” said Dr. Roman. “Taking into account individual risk factors beyond age should allow classification of women into variable risk groups for breast cancer. Personalized risk-based screening that goes beyond the current ‘one size fits all’ recommendation ‘can increase the effectiveness of breast cancer detection Including information from BBD, in addition to other factors, to develop risk-based screening approaches can help predict whether a woman would develop breast cancer within a defined period.
“Different screening strategies can be considered for each woman based on her personal risk of breast cancer: modifying the detection interval, which can be yearly, or every two to three years, the screening method, for example mammography, ultrasound or magnetic resonance imaging, or the age range in which women are invited to participate in screening. “
Dr. Roman and her colleagues believe that these findings will help clinicians understand the different risks associated with BBD and improve the accuracy of breast cancer risk predictions.
In a statement before the conference, Professor Xavier Castells said: “Physicians involved in treating women with BBD could offer specific surveillance strategies considering, in addition to other factors, whether the BBD was found early or on screening tests. In addition, this information will be included in an individualized model that can be used to predict an individual woman’s risk of developing breast cancer in five to ten years. We have tested this in the context of a screening program, which also includes information on breast density, age, family history of breast cancer and mammographic characteristics “.
The team is part of MyPebs: an international randomized controlled trial, funded by the European Union, that investigates whether a risk-based breast cancer screening strategy, based on a clinical risk score, is more effective than standard screening . This international project, which started in July 2019, will recruit 90,000 participants from six countries and follow them for four years.
The co-chair of the EBCC12, Professor Javier Cortes, is a clinical researcher in the breast cancer research program at the Vall d’Hebron Institute of Oncology in Barcelona, and head of the breast cancer program at the IOB Institute of Oncology in Madrid and Barcelona, and was not involved in this research. She commented: “We know that population-based breast cancer screening programs save lives by detecting cancer at an early stage. However, they may raise questions not only about the best way to treat women with cancer who it may never become a problem in their lives, but also what to do with women with benign breast disease.
“No patient wants to have screening mammograms more often than necessary, but patients and doctors want to be sure that if benign breast disease turns into cancer, it can be detected quickly. The results of this study give us useful information that can improve the accuracy of breast cancer risk prediction models so that we can tailor surveillance strategies for patients with this disease. ”
Women in their 40s who get breast screenings save lives
More information:
Abstract no: 15, “Differences in the risk of breast cancer after benign breast disease according to the type of screening”, Lecture session offered: “Are your breasts still at risk?”, Saturday, 16.00-16.45 hrs, Channel 3 (Dr. Román The presentation will be at 4:10 p.m.).[1] The countries participating in the MyPebs trial are: France, Belgium, Israel, Italy, the United Kingdom, and Spain.
Provided by the European Organization for Research and Treatment of Cancer
Citation: Researchers Reveal Which Benign Breast Disease Is Most Likely To Become Cancer (Oct 2, 2020) Retrieved Oct 2, 2020 from https://medicalxpress.com/news/2020-10-reveal-benign-breast -disease-cancer.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no part may be reproduced without written permission. The content is provided for informational purposes only.
[ad_2]