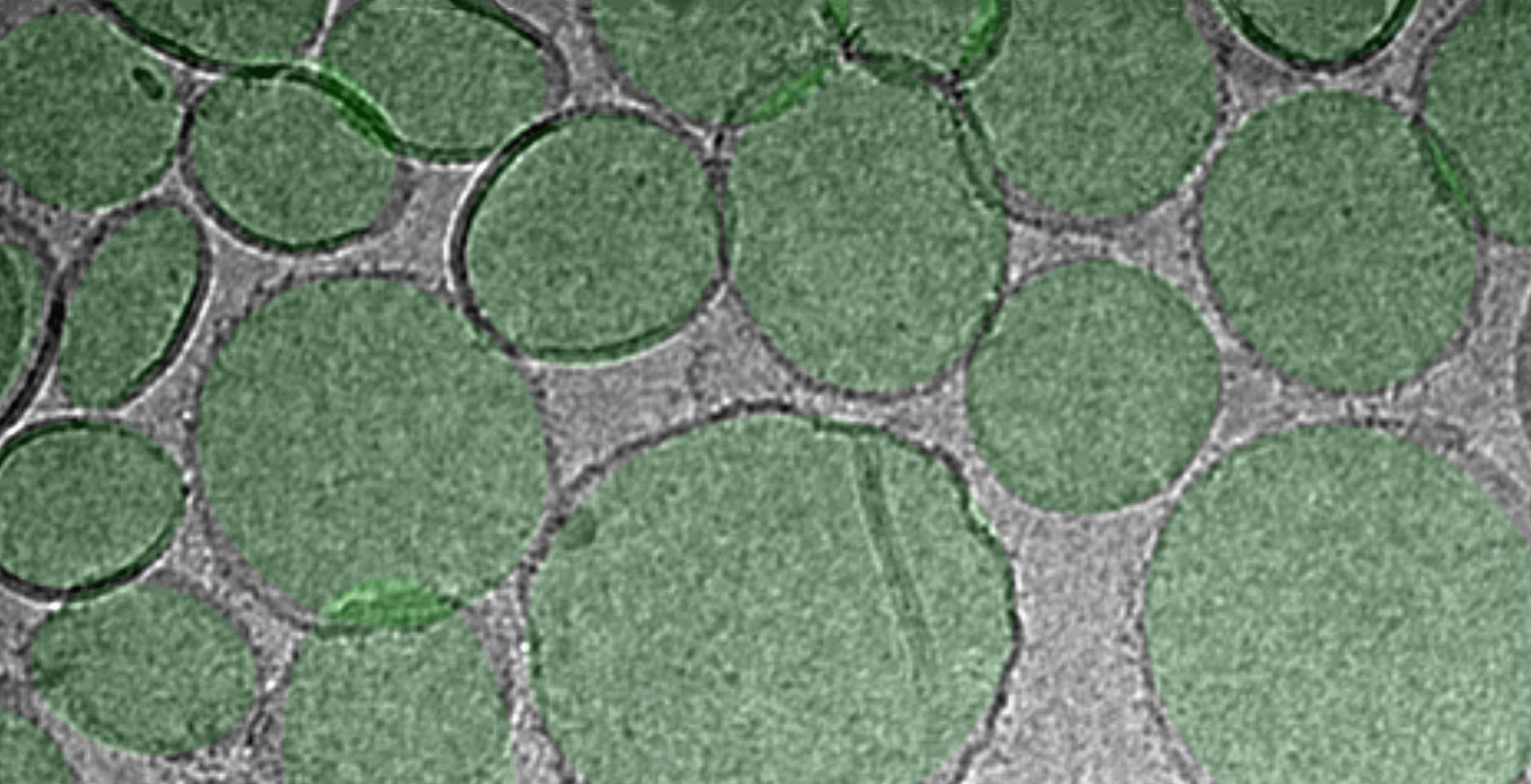

A closer look at the RBD particle vaccine (green). Credit: Facility for Electron Microscopy Research (FEMR) at McGill University
Changing the makeup of a particular protein is likely to neutralize the virus.
a University at Buffalo-The research team has discovered a technique that can help increase the effectiveness of the vaccine against the novel coronavirus, which causes the virus. COVID-19.
Jonathan F. Lovell, PhD, associate professor in the Department of Biomedical Engineering at UB, is the primary investigator on research, entitled “SARS-CoV-2 RBD neutralizing antibody induction is enhanced by particulate vaccination, “which was published online Advanced content Today, October 28, 2020.
COVID-19 has caused a disrupted global epidemic, infecting at least 40 million people worldwide and killing more than 220,000 people in the United States alone. Since its spread began in early 2020, biomedical researchers have been actively pursuing effective vaccines.
According to Lowell, one answer may be in the formulation of vaccines that partially mimic the structure of the virus. One of the proteins on the virus – located on the characteristic COVID spike – contains a component called the receptor-binding domain or RBD, which is its “Achilles heel”. That is, he said, antibodies against this part of the virus are likely to neutralize the virus.
“It’s exciting if a vaccine induces high-level antibodies against RBD,” Lovele said. “One way to achieve this goal is to use RBD protein as an antigen, a component of the vaccine that will be used against the immune response.”
The team hypothesized that by converting RBD into nanoparticles (similar in size to viruses) instead of allowing it to remain in its natural form as a small protein, it would produce antibodies at neutral levels and produce the ability to produce an immune response. Will increase.
Lovell’s team previously developed a technique that facilitates the conversion of small, pure proteins into particles through the use of liposomes or the formation of small nanoparticles composed of naturally occurring fatty components. In a new study, researchers included a special lipid called cobalt-porphyrin-phospholipid or COPOP within liposomes. It enables special lipid RBD proteins to rapidly bind to liposomes, creating more nanoparticles that produce an immune response, Lovele said.
The team observed that when RBD was converted into nanoparticles, it retained its true, three-dimensional shape and the particles were stable in the same incubation state as in the human body. When laboratory rats and rabbits were immunized with RBD particles, higher antibody levels were induced. Compared to other materials combined with RBD to boost immunity, only the Kopop-containing particulate approach reacted strongly.
Other vaccine-assisted technologies do not have the ability to convert RBD into particle-form, Lovele said.
“We think these results provide evidence to the vaccine-development community that the RBD antigen has the great advantage of being in a microcosm,” Lovele said. “This could help future vaccine designs target this specific antigen.”
Reference: “SARS-KOV-2 RBD neutralizing antibody induction is enhanced by particulate vaccination” Wei – Chiao Huang, Shiki Zhou, Zukden Hee, Kevin Chime, Mustafa T. Mab Brock, Ruth H. Nisley, Mike Strauss, Sunshine Sambhara, Jock qu n te rtega, Elizabeth a. Wohlfert, Luis Martinez – Sobrido, Suresh V. Kuchipudi, Bruce A. Davidson and Jonathan F. Love, 28 October October 2020, Advanced content.
DOI: 10.1002 / ADMA.202005637
Lovell’s co-authors on the study include Wai-Chiao Huang, Shiki Zhou, Zukdan Hee, and Mustafa T. Kevin Chime and Luis Martinez-Sobrido of the Texas Biomedical Research Institute; Ruth H. Nisley, Ian M. Bird and Suresh V. Kuchipudi, from the Animal Diagnostic Laboratory, Department of Veterinary and Biomedical Sciences, Pennsylvania State University; Mike Strauss and Joaquin Ortega from the Department of Anatomy and Cell Biology at McGill University; U.S. for Disease Control and Prevention Sunlight retention from the immunology and pathogenesis branch of the centers; Elizabeth A. from the Department of Microbiology and Immunology at UB. Wolfert; And Bruce A. Davidson of the Department of Anesthesiology and the Department of Pathology and Anatomical Sciences at UB.
Lovely founded Lovely Lab at UB in 2012. The novel focuses on developing nanomedicine approaches to meet the unavoidable needs in the treatment and prevention of this disease. That P.O.P. Biotechnologies, Inc. Is also a co-founder of, which produces pay-per-click drug and vaccine products.
The study was supported by Electron Microscopy Research (FEMR) for facilitation at the U.S. National Institutes of Health and McGill University. FEMR is supported by the Canadian Foundation for Innovation, the Government of Quebec, and McGill University.