Coronavirus cases on the rise. Hospitals filling up. Reopening of postponed schools. The battles over wearing masks in public intensify.
July has brought a month of grim COVID-19 headlines to California, with a state that was once seen as a prevention model that supports a further surge in cases as the economy quickly reopened.
But will July end with more bad news or some tentative signs that efforts to curb infections by shutting down some companies and institutions may be paying off?
Health officials are eager for more signs of the latter, especially amid signs that other critical states may begin to stabilize.
“We are in the phase of starting to flatten the curve, albeit at a higher level than before,” Dr. Robert Kim-Farley, a medical epidemiologist and infectious disease expert at the Fielding School of Public Health in California, said Sunday. UCLA. “I would anticipate, depending on the cooperation of the public, that we would begin to see cases that would begin to decline in the next two weeks.”
Kim-Farley said Sunday that according to information now available, it will not be necessary to close any more businesses, and in about two to three weeks, parts of California may be at a point where some businesses may slowly and slowly reopen. gradual.
The state’s hospital system has not been largely overwhelmed in this latest surge, Kim-Farley said. And where there was a hospital system overwhelmed at a local hot spot, the problem in some cases was a shortage of medical personnel, rather than physical beds. Some of that has been alleviated by transferring patients to other nearby counties and assigning federal doctors and nurses to hospitals in the Central Valley and southern California, she said.
Other critical states are also beginning to show signs of improvement. The rate at which coronavirus test results are yielding positive results is beginning to decline in Arizona and Texas, although “it’s a bit more of a mix in Florida and California,” said Dr. Scott Gottlieb, former chief of the Food and Drug Administration said on CBS “Face the Nation” on Sunday.
“We will have to wait another week to see how those states recover. But there are unequivocal signs that the epidemic appears to be slowing in these states, “said Gottlieb. But he cautioned that the pandemic seemed to be on the rise in other southern states, the Midwest, and the District of Columbia.
In Arizona, the seven-day positivity rate for coronavirus testing was 22%, down from 28% in mid-July, according to the COVID Monitoring Project. A Los Angeles Times analysis found that California’s seven-day positivity rate has generally been between 7% and 8% since July 5. That rate is worse than it was at the end of May, when it was around 4%, authorities say, but at least the rate is no longer on a sustained upward trajectory as it was in June. A higher positivity rate indicates that the spread of the disease is worsening.
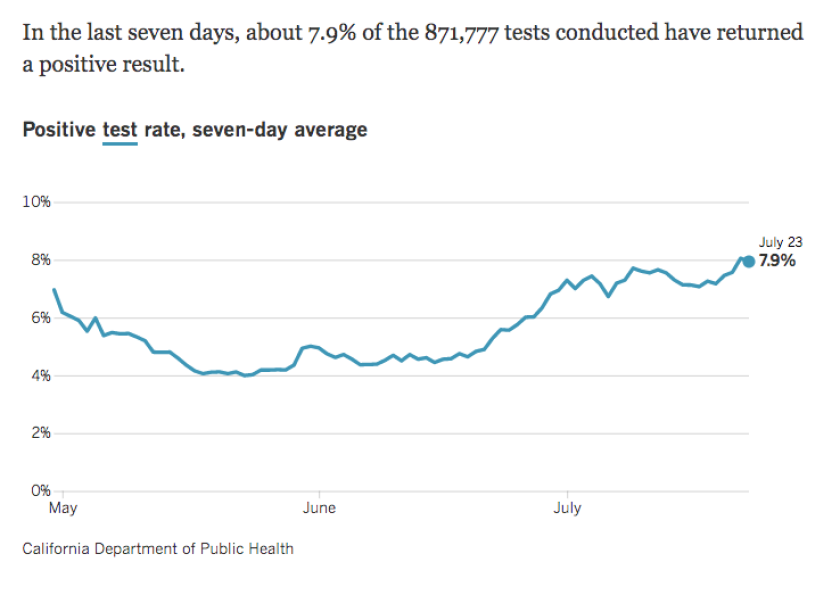
The rate at which the results of the California coronavirus test turn positive has remained more or less stable in recent weeks, between 7% and 8%.
(Los Angeles Times)
In Los Angeles County, the positivity rate has been stable at approximately 8.5% since July 1. It was approximately 4% at the end of May. “The fact that we are leveling out is encouraging,” Barbara Ferrer, director of public health for Los Angeles County, said last week. “We would like to see it fall again.”
There are still worrying numbers across the state. The effective transmission rate of the coronavirus in California ranges from 1.1 to 1.3, which means that each infected person in the state, on average, transmits it to 1.1 to 1.3 people, which sets the stage to worsen the transmission of the disease, according to data shared Friday by California Health and Human Services Agency Secretary Dr. Mark Ghaly.
The transmission rate is now worse in northern and central California than in much of southern California, according to models published by state public health officials. The spread of COVID-19 is likely stable in LA, San Diego, Orange, Riverside, San Bernardino, and Imperial counties, but is likely increasing in Ventura County, the San Francisco Bay Area, and the Central Valley.
Dr. George Rutherford, an epidemiologist at UC San Francisco and an infectious disease expert, presented data Friday at a city council meeting that indicated the transmission rate in San Francisco, Santa Clara, Contra Costa and San Mateo counties was around 1.3 or 1.4. “This is far, far, far from satisfactory,” said Rutherford.
There are also some concerns about the shortage of a key antiviral drug, remdesivir, which has been used to shorten recovery times. The Bay Area “hospitals and many more across the country are starting to run out of #remdesivir,” Dr. Peter Chin-Hong, professor of medicine and infectious disease specialist at UC San Francisco, tweeted.
Last week, California recorded more than 150 deaths on each of those days on Wednesday and Thursday, the worst death toll in a single day since the pandemic began. Deaths tend to be a lagging indicator of an outbreak, and experts say they believe the deaths are related to infections that likely occurred in June when people left their homes en masse and returned to old pre-COVID activities, such as parties. or worked in places that had not instituted new health and safety precautions.
Despite the increase, California has seen far fewer deaths, more than 8,400, from COVID-19 than New York, which has recorded more than 32,000 deaths and was the nation’s worst early critical point. But officials have warned that the situation here could deteriorate rapidly.
San Francisco has remained in what officials called its red zone last week, given its rapid rise in hospitalizations, and officials warned that an overwhelming number of hospitals are still plausible as New York saw it in the spring.
“It is plausible that we may have a situation similar to New York in the late summer or early fall. That’s why everyone should do their part to flatten the curve, ”said Dr. Grant Colfax, director of public health in San Francisco.
The number of new COVID-19 patients requiring hospitalization in Los Angeles County, which had increased, has decreased and may even be starting to decrease, said Dr. Christina Ghaly, director of county health services for The Angels.
It stalled at a substantially worse number than in April, but the data suggests an improvement. The number of ICU beds in Los Angeles County available for use has also been stable, ranging from 130 to 160 beds on any given day.
“I hope this week marks a turning point, and that we begin to see the results of our corrective actions to curb the spread of COVID-19,” Dr. Muntu Davis, the Los Angeles County health officer, said Thursday.
It can take three to four weeks after exposure to the virus for infected people to get sick enough to be hospitalized, and four to five weeks after exposure for some of the most vulnerable patients to die from the virus. disease.
Governor Gavin Newsom said last week that state officials were preparing hospitals for what might come.
At a press conference held in a Sacramento warehouse that houses personal protective equipment, Newsom said Wednesday that it is extending a contract with Chinese firm BYD to buy an additional 300 million surgical masks and an additional 120 million N95 face masks to protect medical workers and others, while he is also seeking offers from companies that may provide protective equipment in the coming months. The so-called bridge contract is worth $ 315 million.
The governor said the move is necessary because California is shipping 46 million masks per month and has an inventory of 111 million N95 masks.
“We were able to turn the curve many months ago in the state of California,” Newsom said. “That gave us time to buy and acquire the type of equipment you see behind me and come up with our plans.”
The California Hospital Association. asks the Newsom administration to seek additional federal aid to provide staff and to reconsider existing relationships between nurses and patients as conditions worsen.
Newsom said the state has a strategy “to address the possibility of increased hospital utilization, the need to develop alternative care sites outside of our hospital system to help isolate and quarantine people.”
The governor acknowledged that he continues to hear complaints from medical workers that they do not receive enough medical masks and other protective equipment despite the increase in deliveries by the state.
She said an advocate for nurses recently told her that many receive only two to three masks per week, although medical standards require more.
“That is unacceptable,” Newsom said. “We still hear those stories and we have to address that problem.”
Lin and Dolan reported from San Francisco, McGreevy from Sacramento.