
Ultimately, the only way that societies can return to a normal appearance in the wake of the current pandemic is to achieve a state called collective immunity. This is where a sufficiently large percentage of the population has acquired immunity to SARS-CoV-2, either through an infection or a vaccine, that most people exposed to the virus are already immune to it. This will mean that the infection rate will decrease and eventually disappear, protecting society as a whole.
Since this is our ultimate goal, we must understand how the immune system responds to this virus. Most of what we know is based on a combination of what we know about other coronaviruses that infect humans and the antibody response to SARS-CoV-2. But now, data on the T-cell response is coming in, indicating that its response is more complex: longer-lasting, broad-based, and includes an overlap with the response to previous coronavirus infections. What this means for the prospect of lasting protection remains unclear.
What we know now
SARS-CoV-2 is one of seven coronaviruses known to infect humans. Some of these, like SARS and MERS, have only made the leap to humans recently. While they are more lethal than SARS-CoV-2, we are fortunate that they spread to humans less efficiently. These viruses appear to elicit a long-lasting immune response after infections. That’s in stark contrast to the four coronaviruses that circulate widely among humans, causing cold-like symptoms. These viruses induce immunity that appears to last less than a year.
We still don’t know much about the immune response to SARS-CoV-2. By tracking antibody production, it is clear that many of those infected have a robust immune response, but “many” is far from “all”, there is a lot of variability in the level of response. This variability is associated with a large difference in COVID-19 severity among patients. One area of concern is that the antibody response to SARS-CoV-2 appears to be decreasing rapidly.
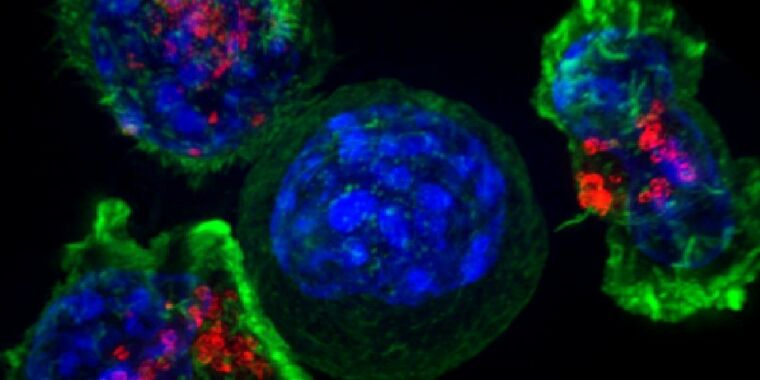
The antibody response, however, is only part of the defense of the immune system against a pathogen. Antibodies generally recognize proteins that reside on the surface of a virus, since those are the cells to which the cells that make antibodies are exposed. But a second group of cells, called T cells, have a different way of recognizing pathogens. T cells are based on a system used by all cells, which takes small pieces of the proteins they make and presents them on the cell surface. Due to how the system works, it has the potential to recognize more proteins produced by a virus, not just those on its surface.
(Some pathogen-swallowing immune cells also place protein fragments on their surface in the same way.)
Once there, any T cell that recognizes these tiny pieces of protein as foreign can mount a variety of responses, from the activation of its partner immune cells to the destruction of the cell that produces foreign proteins. Studying the response of T cells is much more challenging since it relies on cells, rather than antibodies, which are proteins. But such a study may be equally critical to long-term immunity.
Studying the Ts
To study the T-cell response, a group of researchers based in Singapore focused on proteins that are internal to the virus or used only in the cells it infects and are therefore not a primary focus of the response. of antibodies. To verify the response to these proteins, the researchers made a set of 15 amino acid protein fragments that together span the entire length of the protein. They then collected blood cells from people who had recovered from COVID-19, from those who recovered from original SARS, and from those who were never exposed to any of the viruses.
These fragments were pooled and mixed with blood cells to determine if any T cells within them reacted to them. By narrowing the clusters, the researchers were able to identify the specific fragment, and therefore the specific region of the protein it came from, to which the T cells responded. The response was recorded by checking the level of an immune signaling molecule produced. by T cells.
One of the potentially reassuring findings was that people who had been exposed to the original SARS virus 17 years earlier still had T cells that responded to the virus fragments. This was true despite the fact that the antibody response to this virus had generally faded after several years. Less surprising, people who had recently had COVID-19 also had T cells that responded to fragments of the virus’s proteins.
But there was a surprising feature of the SARS and COVID-19 fragments that T cells responded to: many of them were identical. Although SARS-CoV-1 and -2 are distinct viruses with different evolutionary histories, many of their proteins remain extremely similar. (It is probably because they continue to perform similar functions, and therefore there is evolutionary pressure against the changes.) As a result, several of the fragments that were made based on the SARS-CoV-2 proteins were found to be identical in the SARS-CoV-1 equivalent protein. So a T cell that recognized one of these fragments was able to recognize both viruses, even though it came from a patient who had only been exposed to one.
Surprise!
That sets the stage for the study’s most surprising result. Participants who had never been exposed to any of the SARS viruses also had some T cells that recognized fragments of SARS-CoV-2 proteins. This was not true for all participants in the unexposed group; only half of them had these reactive T cells. But, again, it relied primarily on cells that reacted to pieces of protein that were identical between SARS-CoV-2 and the viruses that cause the common cold.
Above all, but not all. There were two exceptions to this: Two protein fragments that did not resemble the cold virus, but elicited a T-cell response from the unexposed participants, and the researchers struggle to explain them. Their only suggestion is that some other pathogen happens randomly to have a small section of protein that looks like this. There were also differences between groups regarding which of the three proteins their T cells recognize, but the significance of these differences is unclear.
What does this all mean?
So does this mean that the common cold can protect some of us from COVID-19? There is no way of knowing based on these results. Previous exposure to cold-causing coronaviruses appears to induce a different protein response to exposure to SARS-CoV-2. And there is no indication that antibodies to the common cold viruses cross-react with SARS-CoV-2. Would a T cell-based response alone be enough to avoid the virus? We do not know
At the same time, the fact that this response is only present in a subset of people who have never been exposed could explain some of the differences in COVID-19 symptom severity. Obviously there is much more work to be done here.
The importance of T-cell based immunity is also critical to understanding the seemingly highly variable antibody response problem, as well as indications that it may disappear rapidly once SARS-CoV-2 infection is eliminated. This study indicates that T cell responses are consistent and strong in this small population. Parallel work in SARS patients indicates that this response also lasts much longer than the antibody-based immune response. So if it is enough to provide protection against reinfection then we might be less concerned with the erratic response of the antibodies. Again, we don’t know yet.
This could also have implications for vaccine development, which tend to focus on the production of neutralizing antibodies.
All of which implies that there is an urgent need to better understand the response of T cells to SARS-CoV-2. Which is unfortunate, given how difficult it is to study T cells.
Nature, 2020. DOI: 10.1038 / s41586-020-2550-z (About DOIs).