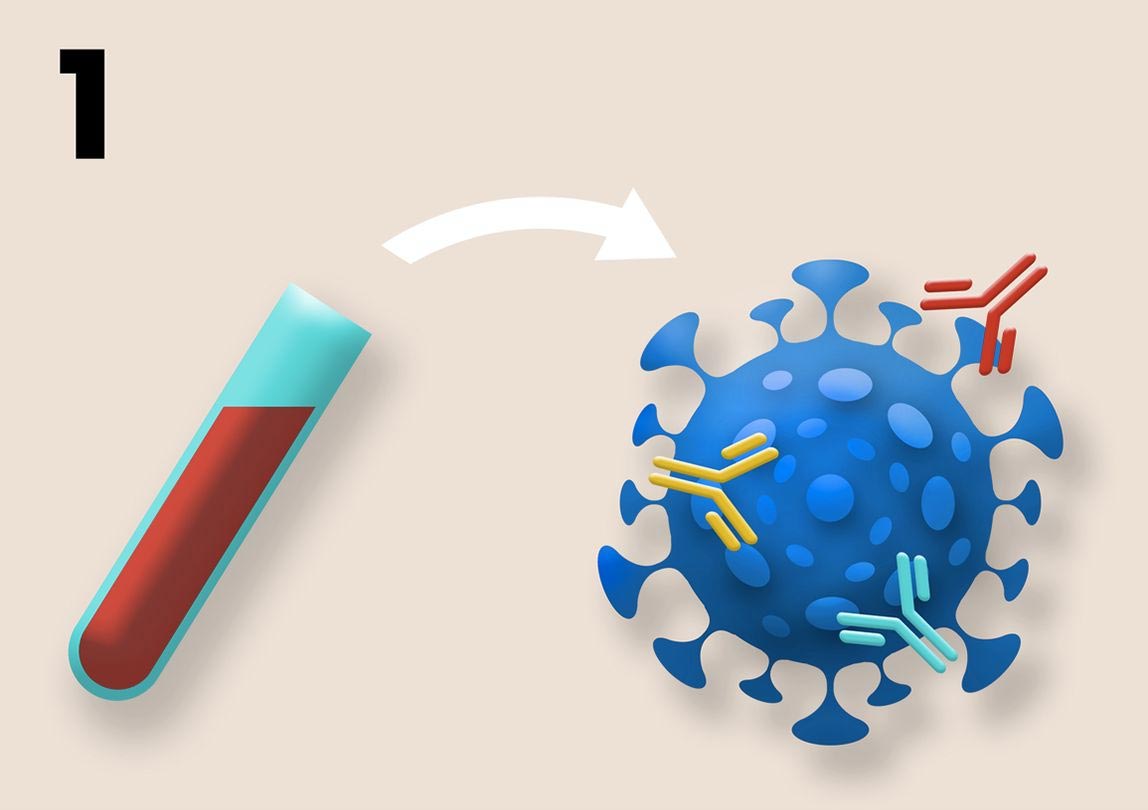

The series of pictures on this page is a schematic description of how standard samples of COVID-19 clinical trials can be reconstructed to assess the risk of developing vaccine resistance. 1. The complexity of B-cell and T-cell responses can be measured using blood samples. Above are shown various neutral antibodies in different colors. More complex responses suggest more evolutionary stronger immunity. Credit: Kennedy et al, 2020 (CC by PLoS Biology, 4.0)
Just like bacteria that develop resistance to antibiotics, viruses can develop resistance to vaccines, and evolution SARS-CoV-2 According to a paper published today (November 9, 2020) in the journal Open-Access Access, the effectiveness of vaccines currently under development may be impaired. PLOS Biology U.S. by David Kennedy and Andrew. Read from Pennsylvania State University. The authors also make recommendations to vaccine developers to reduce the likelihood of this outcome.
“a COVID-19 Vaccines are urgently needed to save lives and bring society back to normal in its epidemic, ”said David Kennedy, an assistant professor of biology. “As we have seen with other diseases like pneumonia, the evolution of resistance can quickly make the vaccine ineffective. By learning from previous challenges and applying this knowledge during vaccine design, we will be able to maximize the long-term effects of COVID-19 vaccines. “

2. The effect of vaccination on transmission potential can be assessed by collecting viral titer data using regular nasal swabs. Plaque aces from multiple vaccination and control individuals are compiled into histograms. Due to the absence of complete immune protection or exposure, undiagnosed viral titers indicate a low or no chance of infection. High viral titers indicate high transmission potential due to the absence of a protective immune response. Intermediate viral titers, marked with an asterisk above, indicate moderate transmission potential due to partial vaccine protection. Intermediate titers indicate an increased risk for immune evolution because pathogen diversity can be generated within hosts and act during transitions between selected hosts. Credit: Kennedy et al, 2020 (CC by PLoS Biology, 4.0)
Researchers have specifically suggested that standard blood and nose-swab samples taken during clinical trials to quantify people’s responses to vaccinations may also be used to assess the likelihood that vaccination will lead to resistance evolution. For example, the team proposed that blood samples could be used to evaluate the immunity produced by a candidate’s vaccine, to measure the types and amounts of antibodies and T-cells present.
“How antibiotic therapy delays the evolution of antibiotic resistance, such as vaccines, designed to induce an unwanted immune response – or one in which the immune system is stimulated to target multiple sites called epithelial surfaces – , May delay. The evolution of vaccine resistance, ”said Andrew Reed, Evan Pug Professor of Biology and Entomology and director of the Institute for the Rights of Life Sciences. “That’s because the virus has to undergo many mutations against just one gene to survive the attack of the host immune system.”

Vacc. Values of pre-existing variations for vaccine resistance can be obtained by obtaining genome sequences from the nasopharyngeal swabs of typical COVID-19 cases included in the study. In placebo-controlled, double-blind studies, significant differences in the genome sequences of vaccinated and controlled individuals samples indicate at least partial vaccine resistance. Credit: Kennedy et al, 2020 (CC by PLoS Biology, 4.0)
Researchers have also recommended that nasal swabs commonly collected during clinical trials be used to determine the amount of viral titer or virus present, which is considered a proxy for transmission potential. They note that strongly suppressing the transmission of the virus by vaccinated hosts is key to slowing the evolution of resistance, as it also reduces the chances of mutations occurring and the chances of natural selection to act on the mutations that occur.
In addition, the team suggests that genetic data obtained through nasal swabs can be used to investigate whether a vaccine-based selection has been made. For example, differences between the viral genomes collected from unvaccinated individuals versus vaccinated indicate differences in the types of genes arising from alleles or mutations indicate that selection has taken place.
“According to the World Health Organization, at least 198 Covid-19 vaccines are in the development pipeline, of which 44 are currently undergoing clinical evaluation,” Kennedy said. “We suggest that resistance risk is used to prioritize investment in otherwise equally promising vaccine candidates.”
Ref: 9 November 2020, PLOS Biology.
DOI: 10.1371 / journal.pbio.3001000