[ad_1]
The NHS 111 service has permanently detained nurses and other health professionals who take clinical calls with people suspected of having Covid-19 after an audit of the recorded calls found that more than 60% were unsafe.
The audit began in July after many of the medical professionals recruited to work in the 111 clinical division sounded the alarm, saying they did not feel “properly trained and competent” to fulfill such a critical role.
An investigation into several individual cases was launched after the initial review determined that no guarantees could be given “regarding the safety of these calls,” according to an email, seen by The Guardian, from the National Covid director of clinical assurance. – 19 Pandemic response service. In another email on Aug. 14, he told staff that after hearing a “significant number” of calls “so far over 60% … have not passed the criteria for a secure call.”
Several “clinical incidents” were being investigated, he said, because some calls “may have resulted in damage.” One case had been “escalated as a serious adverse event with potential harm to the patient.”
NHS England declined to answer questions about any aspect of these apparent security flaws, saying it was the responsibility of the South Central Ambulance Service (SCAS), which created a section of NHS 111 called the Covid-19 Clinical Assessment Service (CCAS). CCAS staff are responsible for calling people whose potential Covid-19 symptoms are identified by 111 as severe enough to necessitate a conversation with a doctor.
SCAS declined to say how many calls had been audited and found they were unsafe or to provide information on the outcome of investigations into possible harm to patients. She said Nurses and Allied Health Professionals (AHPs), which included paramedics and physical therapists, initially accounted for just 4% of CCAS’s workforce, and it now has more than 1,600 GPs and medical staff.
An AHP who signed up with CCAS told The Guardian that the clinical calls involved making critical decisions about whether a person was in a life-threatening condition and needed immediate emergency care. Their training and experience had never involved emergency care, they said, adding that they did not feel qualified for the position and were “appalled” by the outcome of the audit of the call.
The apparent failures of the NHS 111 clinical division are likely to reinforce calls from families whose relatives died from Covid 19 for an immediate public investigation into the performance of the 111 service.
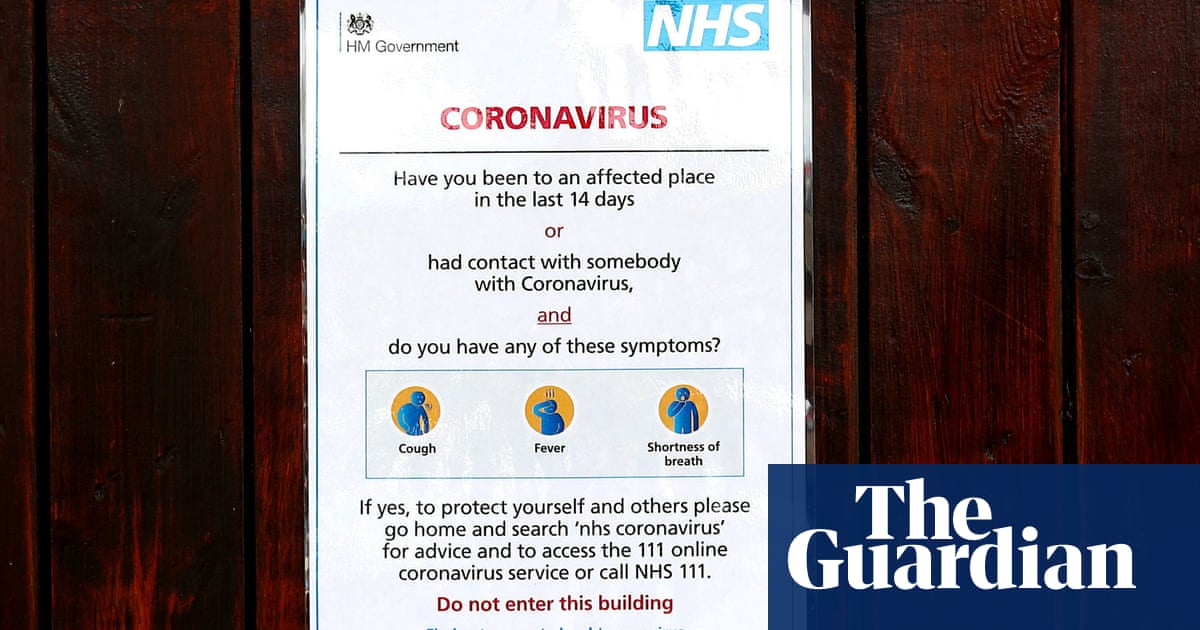
At the height of the pandemic, the government ordered the public to call 111, rather than contact their GPs or go to hospitals, as a strategy to avoid overwhelming doctors and emergency departments. Nearly 6,000 people were quickly recruited to handle calls for a dedicated operation within 111, the Coronavirus Response Service (CRS). For the most part, the CRS was integrated and operated by private corporations contracted by the SCAS on behalf of the NHS.
The Covid-19 Bereaved Families for Justice group says hundreds of its members’ family members called 111, according to instructions, when they were seriously ill but did not receive proper counseling, and some were told to stay home and take acetaminophen. and then died shortly after. .
NHS England and SCAS told The Guardian in statements that call managers for the CRS were “carefully selected, screened and trained.”
However, The Guardian interviewed three people working for 111 at different sites in England and they say they were given the job after a relatively brief conversation with a recruiting agent and negligible training. Two worked for the French company Teleperformance at call centers in Gateshead and Ashby, and the other for the French-American call center giant Sitel at a site in Newcastle.
The two employees who worked for Teleperformance said they only had an induction session on their first morning, which was primarily about the company they were working for and the building, and involved minimal training in Covid-19 symptoms or handling. calls from the public. Ashby’s manager said that when he started working he didn’t even know how to operate the phone system.
In normal times, NHS 111 call handlers have a minimum of six weeks of full-time training, including classroom learning and call center training. A job description seen by The Guardian sets out 33 main duties and responsibilities, including operating the NHS Pathways computer system that classifies people according to clinical needs and speaking confidently with distressed, sometimes abusive patients in “situations of protection or life threatening under pressure “. .
This level of training and clinical governance was not necessary for new recruits to Service 111 during the pandemic.
The Teleperformance employee in Gateshead said that on the same floor where 111 calls were being handled, the company was handling calls for clothing company Asos. They said they were told to follow a flow chart in a Word document that explained how to handle 111 calls. It asked about people’s symptoms and led to a result, they said, adding that it generally concluded that they should stay home if they had symptoms, unless they had acute shortness of breath.
Sitel did not respond to questions from The Guardian. A spokesperson for Teleperformance said their service included call managers providing “standard information based on NHS scripts” and that all employees “received a training program designed in accordance with NHS guidelines.”
“It’s a joke to say we had a training program,” said the Teleperformance employee in Gateshead. “I didn’t even have time to read the flow chart before I started taking calls. The first call I had, the person was distraught. The flow chart gave rise to the advice that you should stay home and rest. It was frightening; many young people were hired, some were not taking it seriously. It breaks my heart to read about these families whose loved ones died after calling 111. “
SCAS said CRS call handlers used an algorithm based on the NHS Pathways system. “The algorithm that the call controllers used was updated with approved changes in accordance with advice from Public Health England, as we learned more about the virus and its symptoms.” The algorithms were now “more robust as a result of learning in wave 1 of the pandemic,” explained the SCAS.
Jo Goodman, co-founder of the group for grieving families, said: “The revelations about the NHS 111 service are truly shocking and upsetting for anyone who has lost a loved one to the pandemic. The more we listen, the clearer it becomes that those who receive calls from people in life and death situations were terribly ill-prepared for that crucial role. As cases increase, we have to ask ourselves if any lessons have been learned to ensure that this does not happen again. “
Labor MP Kate Osamor, an activist for 111 service reform even before the pandemic, said there had been “a major government failure” and called for a full and independent public investigation.