One of the conspiracy theories that has plagued attempts to keep people informed during the pandemic is the idea that the coronavirus was created in a laboratory. But the vast majority of scientists who have studied the virus agree that it evolved naturally and crossed humans from an animal species, likely a bat.
How exactly do we know that this virus, SARS-CoV-2, has an “zoonotic” animal origin and not an artificial one? The answers lie in the genetic material and evolutionary history of the virus, and in understanding the ecology of the bats in question.
An estimated 60 percent of known infectious diseases and 75 percent of all new, emerging, or reemerging diseases in humans have animal origins. SARS-CoV-2 is the newest of the seven coronaviruses found in humans, all of which come from animals, be it from bats, mice, or pets.
Bats were also the source of the viruses that cause Ebola, rabies, Nipah and Hendra virus infections, Marburg virus disease, and strains of the Influenza A virus.
The genetic makeup or “genome” of SARS-CoV-2 has been sequenced and publicly shared thousands of times by scientists around the world. If the virus had been genetically modified in a laboratory, there would be signs of tampering in the genome data.
This would include evidence of an existing viral sequence such as the backbone of the new virus and obvious genetic elements inserted (or removed).
But there is no such evidence. It is highly unlikely that the techniques used to genetically modify the virus will not leave a genetic signature, such as specific identifiable pieces of DNA code.
The SARS-CoV-2 genome is similar to that of other bat coronaviruses, as well as that of pangolins, all of which have a similar general genomic architecture. The differences between the genomes of these coronaviruses show typical natural patterns of coronavirus evolution. This suggests that SARS-CoV-2 evolved from a previous wild coronavirus.
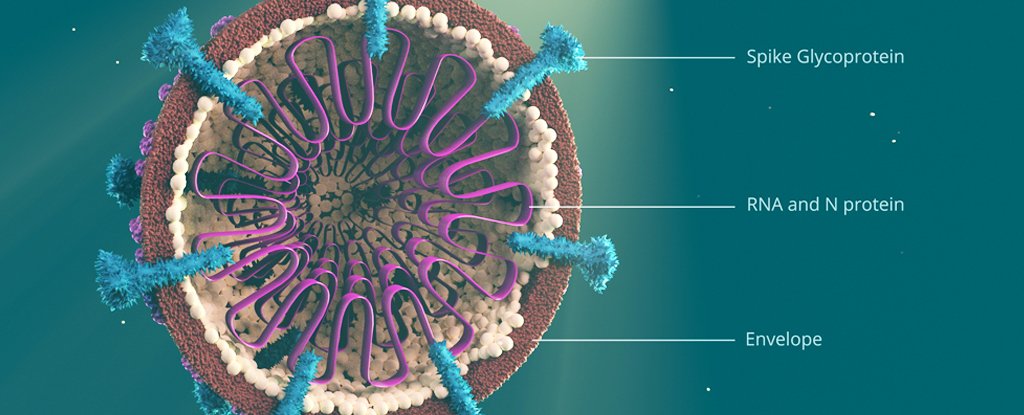
One of the key features that differentiates SARS-CoV-2 from the other coronaviruses is a particular “spike” protein that binds well with another protein on the outside of human cells called ACE2. This allows the virus to latch on and infect a variety of human cells.
However, other related coronaviruses have similar characteristics, providing evidence that they have evolved naturally rather than being artificially added in a laboratory.
Coronaviruses and bats are locked in an evolutionary arms race in which viruses constantly evolve to evade bats’ immune systems, and bats evolve to resist coronavirus infections. A virus will develop multiple variants, most of which will be destroyed by the bat’s immune system, but some will survive and pass to other bats.
Some scientists have suggested that SARS-CoV-2 may come from another known bat virus (RaTG13) found by researchers at the Wuhan Institute of Virology. The genomes of these two viruses are 96% similar to each other.
This may sound very close, but in evolutionary terms, this makes them significantly different and the two have been shown to share a common ancestor. This shows that RaGT13 is not the ancestor of SARS-CoV-2.
In fact, SARS-CoV-2 probably evolved from a viral variant that was unable to survive for a long period of time or that persists at low levels in bats.
Coincidentally, the ability to invade human cells evolved and it accidentally made its way to us, possibly through an intermediate animal host, where it later thrived. Or an initially harmless form of the virus could have leaped directly into humans and then evolved to become harmful as it passed between people.
Genetic variations
The mixing or “recombination” of different coronavirus genomes in nature is one of the mechanisms that produces new coronaviruses. There is now more evidence that this process could be involved in the generation of SARS-CoV-2.
Since the pandemic began, the SARS-CoV-2 virus appears to have begun to evolve into two different strains, acquiring adaptations for a more efficient invasion of human cells. This could have happened through a mechanism known as selective scanning, through which beneficial mutations help a virus infect more hosts and thus become more common in the viral population.
This is a natural process that can ultimately reduce genetic variation between individual viral genomes.
The same mechanism would explain the lack of diversity observed in the many SAR-CoV-2 genomes that have been sequenced. This indicates that the ancestor of SARS-CoV-2 could have been circulating in bat populations for a considerable time. He would then have acquired the mutations that allowed him to pass from bats to other animals, including humans.
It is also important to remember that around one in five species of mammals on Earth are bats, some found only in certain places and others migrated over great distances. This diversity and geographic extent makes it challenging to identify which group of bats SARS-CoV-2 originally came from.
There is evidence that the first cases of COVID-19 occurred outside of Wuhan in China and did not have a clear link to the city’s wet market where the pandemic is believed to have started. But that is not evidence of a conspiracy.
It could simply be that infected people accidentally introduced the virus into the city and then into the wet market, where closed and busy conditions increased the chances of the disease spreading rapidly.
This includes the possibility that one of the scientists involved in bat coronavirus research in Wuhan would unknowingly become infected and bring the virus from where his bats lived. This would still be considered a natural infection, not a laboratory leak.
Only through sound science and the study of the natural world can we truly understand the natural history and origins of zoonotic diseases like COVID-19. This is relevant because our ever-changing relationship and increasing contact with wildlife increases the risk of new deadly zoonotic diseases that arise in humans.
SARS-CoV-2 is not the first virus we have acquired from animals and it certainly will not be the last. ![]()
Polly Hayes, Professor of Parasitology and Medical Microbiology, University of Westminster.
This article is republished from The Conversation under a Creative Commons license. Read the original article.
.