[ad_1]
The COVID-19 pandemic has spread to 210 countries. As of April 30, more than 3.2 million people had tested positive for the virus and 228,239 people had died.
Many reports circulate about possible drugs, causing confusion among the public.
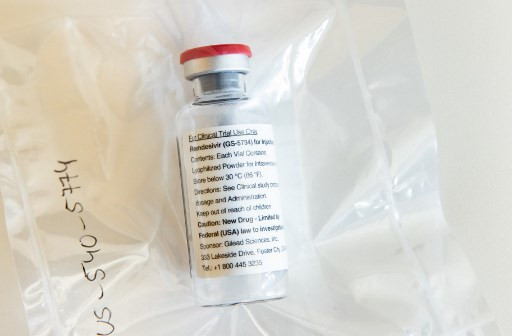
Various types of medications are being studied to treat COVID-19. Most drugs are antiviral drugs that have been used previously for other conditions. Antiviral drugs include favipiravir, or Avigan, which was used to treat influenza in Japan; remdesivir, which was tested in Ebola; ritonavir-lopinavir, an antiviral medication given to patients with HIV; and ribavirin, which is used for hepatitis C and other viral hemorrhagic fevers.
The Food and Drug Monitoring Agency (BPOM) has published its recommendations for COVID-19 therapy in Indonesia. In Indonesia, the antiviral therapy that is administered to patients with moderate and severe symptoms is favipiravir.
Other countries and the World Health Organization have not yet published specific guidelines on COVID-19 drug treatments, but we can see that several antiviral drugs are being used in other countries. The most common are favipiravir, remdesivir, lopinavir-ritonavir, and ribavirin.
Favipiravir and remdesivir work against viruses by inhibiting RNA-dependent RNA polymerase (RdRP), an enzyme that viruses need to replicate their genetic material in human cells. Ribavirin also works by inhibiting RdRP and interfering with the replication of viral genetic material in other ways. Furthermore, ribavirin was also shown to increase the immunity of human cells to viruses.
Lopinavir-ritonavir was found to hinder the activity of a type of protease that viruses need to replicate.
Virus replication is directly related to the severity of the disease. The data suggests that an increased viral load in SARS-CoV-2, a measure of the amount of virus in a patient’s body, is linked to more severe symptoms. Therefore, the more we can inhibit viral replication and cause a lower viral load, the more we can alleviate the severity of the disease.
Favipiravir, remdesivir, lopinavir-ritonavir and ribavirin have been shown to be effective against SARS-CoV-2 in vitro, which means in laboratory tests with cell cultures. To date, there is no strong evidence that any drug is effective against the virus in humans, regardless of the few case studies that claim the treatments were effective in patients.
Several ongoing clinical trials of antiviral drugs are expected to wrap up by the end of the year. Only then can we obtain more evidence on which drugs, if any, effectively treat COVID-19.
Medicines used to treat other diseases are also being studied to treat COVID-19. These are chloroquine (CQ) and hydroxychloroquine (HCQ). These reused medications have been used to treat malaria and chronic inflammatory diseases. HCQ is a derivative of CQ with less toxic effects than CQ.
Also read: Indonesia meets to keep COVID-19 vaccines affordable drugs
In vitro studies suggest that both CQ and HCQ are efficient in inhibiting SARS-CoV-2. Both drugs prevent the entry of the virus and modulate the immune system. Clinical trial data for both drugs is still limited and inconclusive given small sample sizes with poorly controlled or uncontrolled clinical trials. Numerous randomized control trials are ongoing to establish the effectiveness of these drugs on COVID-19. Despite the lack of compelling evidence to support the use of CQ, China’s medical advisory board has suggested its inclusion in the treatment guidelines, making CQ the first drug used in China and abroad to treat cases. moderate to severe COVID-19.
Type 1 interferons (IFN) are another potential candidate. IFNs are normally produced by our bodies in response to viral infections. Therefore, IFNs have general antiviral properties. Previously, IFNs were investigated for the treatment of Middle East Respiratory Syndrome (MERS).
The MERS virus belongs to the same genus as the SARS-CoV-2: the betacoronavirus. The close relationship between these viruses is the basis for the use of IFN to treat COVID-19. Although current Chinese guidelines list interferons as an alternative to combination therapy, the research results are conflicting and no clinical trials have been completed so far.
Monoclonal antibodies against interleukin-6, a protein produced by various cells to trigger inflammation, have also been used as complementary therapy in China and Singapore.
Known as tocilizumab, these antibodies are administered to alleviate the “cytokine storm” that causes deep damage to the lungs and other organs in patients with COVID-19. In several case reports, this treatment was found to be successful in COVID-19 patients who experienced severe forms of the disease. A small uncontrolled study reported clinical improvement in 91 percent of patients. More clinical studies are underway to confirm this finding.
Due to the lack of clinical trials with these drugs, they can only be administered to patients with COVID-19 under close medical supervision.
Another treatment uses convalescent plasma: plasma drawn from the blood of patients recovered with COVID-19. This plasma contains antibodies that neutralize SARS-CoV-2.
A preliminary study showed that a single 200 milliliter dose of convalescent plasma administered to COVID-19 patients with severe forms of the disease showed promising results. Therefore, a large clinical trial in the United States is underway. The Food and Drug Administration is encouraging recovered patients to donate their blood to support the study. Actor Tom Hanks reportedly offered to donate his blood plasma after his recovery from COVID-19.
The information above is important for people to know and understand so that they can classify the information available. Not everything that goes around is true, and websites can exaggerate the information with an attractive title. For a drug to be approved for human use, the drug must undergo rigorous testing through in vitro studies, preclinical animal testing, and clinical studies to demonstrate its safety and efficacy.
***
Professors of the Pharmacy Studies program of the Indonesian International Institute of Life Sciences (i3L)
Disclaimer: The opinions expressed in this article are those of the author and do not reflect the official position of The Jakarta Post.
If you want to help fight COVID-19, we’ve compiled an updated list of community initiatives designed to help medical workers and low-income people in this article. Link: [UPDATED] Anti-COVID-19 initiatives: helping Indonesia fight the outbreak
[ad_2]