[ad_1]
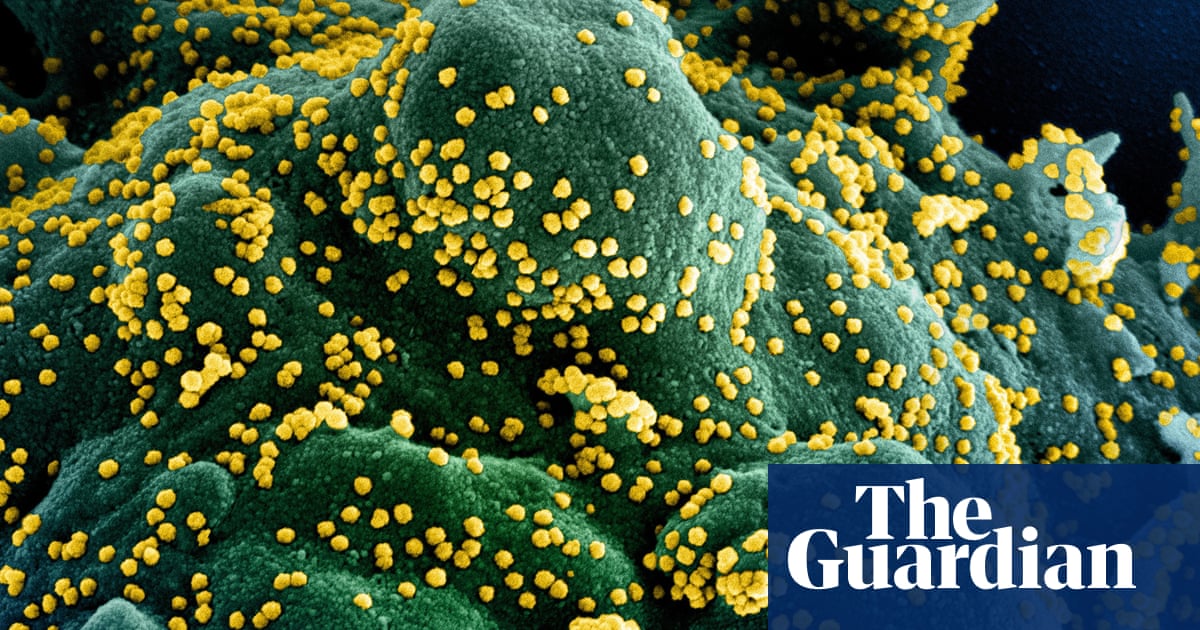
Respiratory physician Dr. David Darley says something peculiar happens to a small group of Covid-19 patients on day seven of their symptoms.
“Until the end of the first week, they are stable,” says Darley, a physician at St Vincent Hospital in Sydney. “And then suddenly they have this hyperinflammatory response. The proteins involved in that inflammation begin to circulate in the body at high levels. “
In these patients, the lungs begin to fight. Low blood pressure. Other organs, including the kidneys, may begin to shut down. Blood clots form throughout the body. The brain and intestines can also be affected. Some suffer changes in their personality, which suggests brain damage.
“I think what is evolving is a very specific set of stages of the disease and for some reason not everyone goes through all the stages,” says Darley. “Some go to the most severe stage and require respiratory support and oxygen. These patients who are severe tend to be older, more likely to be men, and also have other medical problems like diabetes, high blood pressure, or cardiovascular disease. “
But there is no way of knowing which patients will be affected by the most severe symptoms. Doctors like Darley expect a biomarker of disease, a unique characteristic in blood, body fluids, or tissues, to be discovered for each stage.
“It would help doctors predict what stage patients are in and perhaps even if they will progress to the next stage of the disease,” he said. “It could help us predict who needs to be watched more closely in hospitals and it would mean that we have all the systems ready to go if they get worse. And it would give us more confidence to have them discharged at home if a biomarker says they are at low risk of developing serious illness. “
Darley is one of the researchers working on a long-term Saint Vincent study of patients admitted to the hospital with Covid-19. Patients will be followed for one year after discharge, they will be tested at regular intervals to see if there are any lasting effects or changes in the body’s immune system and blood. Continuous changes in lung, bowel, and brain functions will also be evaluated. No It is still unknown whether the virus causes permanent or long-term damage.
“I don’t think it’s clear yet if it’s the virus that infects the lungs and blood vessels, or if it’s the body’s immune system that goes haywire and then causes injury to the lungs and blood vessels,” Darley said. “Or it could be a combination of both.
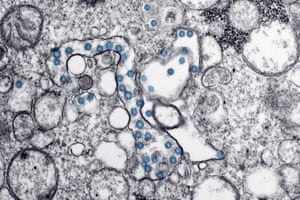
“The pathogenesis is not yet clear. We are observing brain inflammation in a subset of patients, and in those we are seeing agitation and a change in behavior or personality. That’s really interesting, and there are reports from other people, including younger patients, who have a stroke. It is unclear whether the virus is infecting the cells of the lining of blood vessels in the brain, or whether the patient’s blood is excessively prone to clotting due to all the inflammation, leading to a stroke. “
A renowned Italian intensive care specialist, Professor Luciano Gattinoni, said that this type of coagulation in respiratory diseases is “extremely unusual”.
The 75-year-old man has been working in intensive care for 40 years, and said he has never seen anything like what is happening to the lungs of some Covid-19 patients. What is particularly puzzling is that patients have poor oxygenation but little lung damage. This type of presentation is more typical of patients suffering from altitude sickness than a viral infection, says Gattignoni. As a result, patients who are very ill may not feel that they are really struggling to breathe, even when they are critically deprived of oxygen.
“How is this possible?” Gattinoni told Guardian Australia from the intensive care department of the German hospital where he works as a visiting professor. “Poor oxygenation and good lungs tell me that this must have something to do with blood vessels. But these glasses are everywhere. In the brain. In the kidneys So, in some patients, many organs are affected. “
The problem is that mechanical ventilation in intensive care replaces the strength of the respiratory muscles. If patients have difficulty breathing but their lung structure is fine, this ventilation helps little and can actually be harmful, Gattinoni said, because mechanical ventilation is invasive.
He said that while only a small number of patients are severe enough to require ventilation, a significant proportion of those who use ventilators die and continue to show low blood oxygen levels despite mechanical assistance.

Gattinoni said doctors should use ventilators only when necessary and at the right time. Doing this well may improve survival rates, he believes, and he believes that incorrectly scheduled ventilation is the reason why some intensive care units treating patients with Covid-19 have higher mortality rates than others.
“The timing with this disease is absolutely critical,” he said. “Ventilation cannot start too early or too late.” Meanwhile, patients receive blood thinners, medications that prevent or delay blood clotting in the hope that stroke can be prevented.
Darley said the lung scans of Covid-19 patients are unique and show “ground glass opacity,” a confusing pattern that doesn’t hide the underlying lung structure. Lung cancer, for example, usually shows up on a scan as a dark, solid lesion, which obscures other structures in the lungs. While other diseases, for example bacterial infections, can result in opaque ground glass in one scan, there were some unusual features in the scans for Covid-19, Darley said.
“It has a classic pattern at Covid,” he said.
He suspects that men are more severely affected than women because the virus is activated by an enzyme controlled by androgens, a group of hormones that play a role in male characteristics. But more research is needed to test this hypothesis. Darley added that any research on the virus must be done ethically and with sound scientific protocols.
“Without treatment for this virus, all we can do for critically ill patients right now is provide supportive care,” he said. “If the liquid level is low, we can replace it. If they need ventilation, we can help them breathe. But treatments for this disease can only come from clinical trials.
“Our commitment at our hospital is to work with the highest level of scientific research. People are desperate for treatments, but we are reluctant to try treatments outside of clinical trials here.
“If we don’t clearly show that one treatment is better than placebo or other treatments, we could be creating noise and adding to the current chaos in the scientific community.” Our responsibility is to find treatments that work. “
Gattinoni agrees. He said scientists had been trying for decades to find drugs that moderate the inflammatory reaction, and said these drugs had been “romanticized and popularized” in the race to find treatments for Covid-19.
“But in thousands of experiments over the years trying to block inflammatory responses, we’ve only had a lot of bad results,” said Gattinoni. “Like many other things in medicine, we have to be patient.”