Salk Institute scientist and serious biotech entrepreneur Ron Evans yesterday unveiled new mouse work that could point to a long-sought holy grail for treating diabetes.
The study, published in Nature, involved a new approach to islet transplantation, a therapy for diabetes in which dysfunctional cells for producing insulin on the pancreas are replaced with functional ones. The treatment has been around for a while and new ones are in development, but they are hindered by the fact that patients will reject the cells unless they go on immunosuppressive medications.
But, working with iPSC stem cells and tricks from immunotherapy, Evans and his team developed what they called “immune-evasive” clusters of cells – essentially mini-pancreases. These cells were placed in mice, and certain amounts of insulin were secreted without fire from immune cells, pointing the way to a similar approach in humans.
“Most type 1 diabetics are children and teens,” Evans said in a statement. “We hope that regenerative medicine combined with immune protection can make a real difference in the field by replacing damaged cells with lab-generated human island-like cell clusters that produce normal amounts of insulin on demand.”
Evans, who recently co-founded and sold to Astellas the ‘exercise-in-a-pill’ biotech Mitobridge, and his co-authors are hardly alone in this race. ViaCyte has received significant support from both private donors and the Juvenile Diabetes Research Foundation for its own stem cell-derived islet cell transplant. Flagship also launched Sigilon earlier this year with $ 80.3 million in Series B funding. With Robert Langer’s technology, the company is developing polymers that can contain cells for transplantation. A diabetes program is in the IND engagement phase with Eli Lilly.
Four years ago, Evans and his team decided how to create functional pancreatic beta cells for the first time, using a series of molecular chains to get them to not only produce insulin, but do so in response to glucose, like normal cells. do. But that still left questions about how to move from individual cells to pancreatic-like clusters, and how to get these cells to prevent the immune system from transplanting.
To cluster the cells, Evans’ lab found that a protein involved in embryonic development called WNT4 could trigger the same molecular mechanisms that make the functional beta cells. The addition of that protein led to the creation of 3-D clusters of cells similar to what would be seen in humans. They called them human island-like organoids, as HILOs.
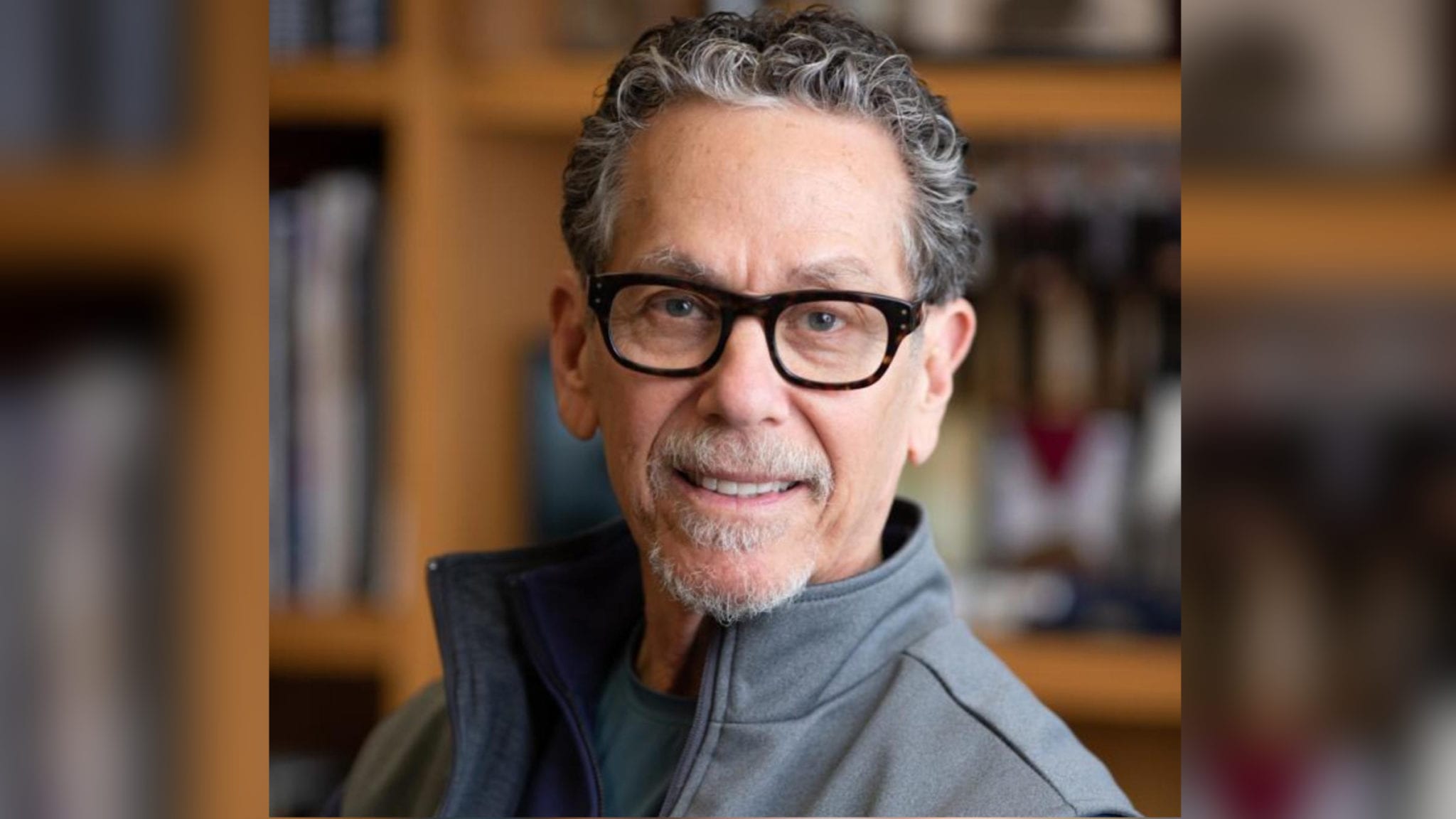
 Evans, with Downes and Yoshihara
Evans, with Downes and YoshiharaTo make those organoids, Evans and Eiji Yoshihara, a scientist in his lab, stole a trick from another field: immuno-oncology. Using short pulses of a protein called interferon gamma, Yoshihara obtained the cells to express PD-L1.
The PD-L1 had the opposite effect of the PD-L1 inhibitors used in cancer. Instead of causing T cells to see a tumor, they prevented T cells from seeing the islet cells.
“This is the first study that shows that you can protect HILOs against the immune system without genetic manipulation,” said Michael Downes, an author on paper. “If we can develop this as therapy, patients will not have to take immunosuppressive drugs.”