In the space of eight months, the new coronavirus SARS-CoV-2 and the disease that causes it, COVID-19, has dominated the work of thousands of researchers in an unusual worldwide effort.
In a series of editorials, we look back at key scientific findings that have revealed key features of the virus and COVID-19, including emerging approaches to treatment and prevention. We begin, this week, with how the virus has been identified; the molecular details of their mechanism of infection; how it is transmitted between people; and the many ways in which it affects the human body.
Crack the virus code
When, in late 2019, an outbreak of a disease similar to severe acute respiratory syndrome (SARS) occurred in Wuhan, China, researchers suspected that a new coronavirus had spread to humans. Many of the first cases identified were linked to a single market for live animals in the city.
Researchers in China immediately began working to isolate and track the virus. When the original SARS virus, now known as SARS-CoV-1, appeared in humans in 2002, it took months to obtain a complete sequence of the virus genome. This time, advances in sequencing technologies meant that scientists were able to erase the RNA code of the virus within weeks of the first cases.
On January 11, Yong-Zhen Zhang at Fudan University in Shanghai and his colleagues deposited the genomic sequence of a virus isolated from a 41-year-old animal that had been working on the animal mark in a public database. In doing so, they warned the world about the existence of a new coronavirus related to SARS-CoV-1. Their findings were later published in Nature1.
Although Zhang’s team had sequences from only one patient, at the same time work by other groups identified the same virus from other people with pneumonia. Together, these researchers implicated this new coronavirus as the cause of the disease. One of the teams, led by Shi Zhengli at the Wuhan Institute of Virology, also determined that the closest known relative of the new virus was a bat coronavirus.2.
Some six months later, the coronavirus destroyed the world. Scientists have now generated more than 80,000 viral sequences. This wealth of genetic information has allowed transmission chains to be traced – public, for example, cryptic community transmission in the United States – as well as showing that a variant that appears to be infectious to cultured cells has now become very dominant.3,4. What this altered infectivity means for transmission and disease is not yet clear.
Not just a respiratory virus
Early reports of the disease, named COVID-19 on February 11, described a severe respiratory disease similar to that caused by SARS-CoV-1. Chest scans showed patchy shadows – known as ‘green glass opacities’ – in the lungs of many patients, according to early studies from hospitals in Wuhan5. In addition, older people, men and people with other illnesses were more often admitted to intensive care, while children had milder illnesses.6.
But it soon became clear that SARS-CoV-2 is not just a respiratory virus. It also affects blood fats, causing thrombosis7 and strokes8. In rare cases, children may develop what is called a multisystem inflammatory syndrome, reminiscent of Kawasaki disease.9.
Autopsies have found the virus in organs other than the lungs, including the kidneys, liver, heart and brain, as well as in the blood.10. We now know that symptoms of COVID-19 can include gastrointestinal, neurological, renal, cardiovascular and other complications11.
Symptoms that different people may experience are thickened by a combination of which cells and tissues are infected; the direct damage that the virus causes to these cells; interference with the normal function of host cells’ ACE2 receptors, where the virus binds; and individual variations in the immune response to the virus. For example, seriously ill patients show hyperactivity of their immune response, which damages the lungs.
Developing these contributions will hopefully lead to effective treatments. The steroid drug dexamethasone, which calms the overactive immune response, has already been shown to reduce mortality from severe COVID-1912. Progress has also been made in managing serious illness. However, what causes the sudden onset of acute respiratory distress in some people is not yet known.
Fashions of infection
A burning question early on was how the new virus infects human cells – the answer would help explain the pathology of the disease, as well as provide clues on how to block infection.
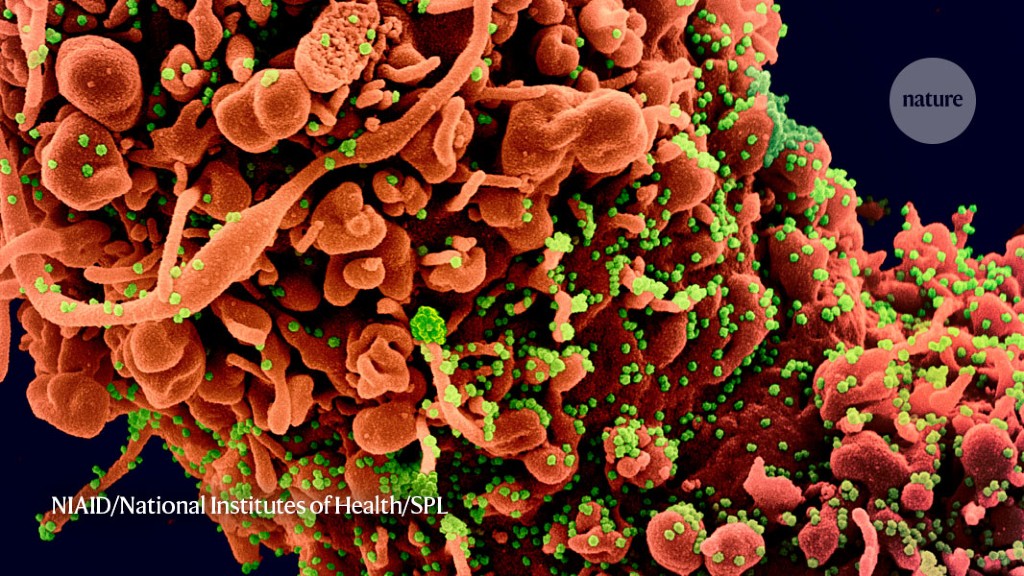
Coronaviruses are decorated with ‘spike’ proteins. This interacts with specific proteins on the surface of the cells that infect them. After binding to the cell receptor, the spike must be cleaved by an enzyme called a protease in the host cell. This activates the spike, which fuses the virus and cell membranes.
Scientists soon showed that both SARS-CoV-1 and the new coronavirus use the same cell receptor, ACE22, and the same protease, TMPRSS213, to enter cells. But SARS-CoV-2 can also infect cell lines that do not express TMPRSS2, which may support drug development.
Researchers used Vero cells – which do not express TMPRSS2 – in an early study that suggested the drug chloroquine might work as a treatment for COVID-1914. But chloroquine proved ineffective in clinical trials, and scientists discovered that it does not inhibit the virus in lung cells expressing TMPRSS215.
Despite the general structural similarity between the spike proteins of the two SARS coronaviruses, scientists found that the SARS-CoV-2 spike binds the ACE2 receptor at least ten times more tightly than SARS-CoV-1 does.16. This may explain some of the differences between how the two viruses infect humans and cause disease.
The SARS-CoV-2 spike also has a function that SARS-CoV-1 lacks: a sequence of amino acids through which it can be recognized and cleaved by an enzyme called furin17. How this sequence contributes to the virulence of SARS-CoV-2 is not yet known. But similar sequences are also found in the receptor-binding protein of some influenza viruses, and contribute to their virulence.
Something in the air
It soon became clear that SARS-CoV-2 could jump from one person to another. This can happen through direct contact or indirect transmission, such as through droplets expelled during a cough, or even a simple exhalation. What was not clear – and is still a matter of debate – is how big those drops should be, and how far they can travel.
It is an important question. Larger droplets will soon fall to the ground, but smaller, lighter ones – known as aerosols – can hang in the air. A virus that can travel on such small droplets can travel further and can increase the risk of infection in poorly ventilated indoor spaces.
The potential of the new coronavirus to travel in this way was the focus of a study, published in April, on SARS-CoV-2 aerodynamics in two hospitals in Wuhan18. Researchers found that some hospital areas, particularly some staff areas, had relatively high concentrations of viral RNA in aerosol-sized droplets.
The team did not determine if those drops were infected, but a US-based team reported in April that both SARS-CoV-2 and SARS-CoV-1 were stable and contaminating in artificially generated aerosols for three hours.19.
It has not yet been definitively shown that SARS-CoV-2 spreads in this way, in part because it is difficult to measure separately the different ways in which it transmits the virus.
Invisible disease
When the virus began to spread around the world, there were suggestions that people without symptoms might be able to transmit it.
In March, data from the cruise ship Diamond Princess showed that 17.9% of those who tested positive for COVID-19 on the ship had no symptoms20. More than 3,700 people were quarantined on board the ship in February after it was revealed that a former passenger had COVID-19. In April, a study of 94 people showed that ‘viral contamination’ – the release of a virus into the environment – seems to peak before or at the same time as the onset of symptoms21. The researchers also evaluated 77 pairs of people, one of whom was probably infected by the other, and found that 44% of the infections were transmitted before the participants developed symptoms.
Which proportion of virus carriers did not show symptoms is still a matter of debate, but it is clear that people can transmit the virus even when they are not sick, which is likely to contribute to its spread.
We have come a long way in getting to know how the pandemic originated and how it spread around the world – by studying the characteristics of the virus and its transmission, and how it causes disease. In future installations by this editorial team, we will look at the research into how it can be checked, as well as advances on treatments and faxes.
