
[ad_1]
In a few days, researchers plan to solve a medical mystery that threatens to erupt in a great transatlantic battle. Scientists at the University of Oxford say they intend to publish full peer-reviewed data in the journal. Lancet, about the trials they have completed with their Covid-19 vaccine.
The information, they say, should end the growing controversy over the vaccine’s effectiveness and explain the apparent inconsistencies in the trial results. Opponents, most of them Americans, say this is unlikely and insist that new phase 3 trials must now be restarted from scratch to restore confidence in the vaccine.
An international vaccine battle has begun, one that will likely be repeated many times over the next year as new vaccines are produced that compete to help rid the world of Covid-19 and doctors try to assess their usefulness. How the Oxford vaccine battle progresses in the coming weeks will have a crucial influence on the global battle against the pandemic.
“The problem is that the Oxford-AstraZeneca vaccine received a lot of publicity over the summer and expectations were high,” said virologist Professor John Moore of Weill Cornell Medicine College in New York. Observer. “These expectations have not been met and now there is a setback.”
On Monday, Oxford researchers announced that their vaccine was 62% effective in most volunteers compared to the recently disclosed efficacy of Pfizer and Moderna vaccines, which exceeded 90%. But they also revealed that a subset of volunteers had been mistakenly given a lower dose of the vaccine due to manufacturing problems. Interestingly, that lower dose produced a higher vaccine efficacy – around 90%. Scientists had no explanation for this anomaly.
“The Oxford vaccine was generally not considered the best design in the world, but it was thought that it might be suitable for its purpose, but now there is a lot of uncertainty,” Moore added. “Other vaccines will be available in the UK and people are likely to want to use the stronger one. It may not be this one. “
Other scientists have defended the Oxford vaccine. Time was a particular issue, said Joy Leahy of the Royal Statistical Society. She said: “The Pfizer and Moderna vaccines produced stronger results than expected. If the Oxford-AstraZeneca data had been published first, I think they would have met the expectations of the scientific community later. “
Professor Helen Fletcher from the London School of Hygiene and Tropical Medicine said it was remarkable that Oxford and AstraZeneca had gone from the starting point of creating 100 million doses of a new vaccine in less than a year, adding: “It is not surprising that some manufacturing problems were still being fixed when clinical trials began. “

The crucial factor is that Covid vaccines work, said Professor Peter Openshaw of Imperial College London. He said: “Each of the trials shows protection, which we did not know would be possible. We have wanted vaccines for many diseases, such as HIV and malaria, and they have not arrived. The results seem to show that it can be done for Covid, and that’s very good news. “
This was endorsed by Kate Bingham, who in May was appointed chair of the UK’s vaccine task force tasked with ensuring Britain received a Covid vaccine as soon as possible. Bingham told the Observer: “Six months ago when we started we were faced with the simple fact that human coronavirus vaccines had never been developed.
“It was overwhelming. Our experiences with other coronavirus vaccines, for both Sars and Mers, had been a failure and many of my colleagues told me it would take years. We now have three candidate vaccines from Oxford-AstraZeneca, Pfizer-BioNtech and Moderna, which have been shown to be highly effective against Covid-19 in clinical trials. What scientists have done is completely amazing. “
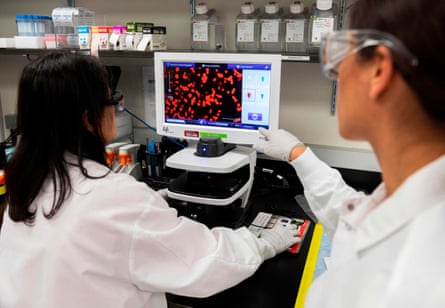
Bingham’s task force spread its bets by seeking and endorsing vaccines that were manufactured using the widest variety of techniques, another factor in the current controversy. Pfizer’s vaccine uses genes from the virus directly to stimulate cells in our bodies to make pieces of Covid protein that trigger immune responses. The AstraZeneca vaccine uses another virus to carry those genes into the body.
Others use inactivated Covid viruses to stimulate immune responses, while the US firm Novavax uses a remarkable technique that involves genetic engineering of cells taken from moths to manufacture pieces of coronavirus protein that will stimulate anti-Covid responses when injected.
Interestingly, Novavax was facing gloomy times in early 2020 after the failure of two different vaccine trials using similar technology. Then came the pandemic, and his moth cell technique quickly transferred to the production of the Covid-19 vaccine. The first trials yielded strong results, and since then Novavax has attracted more than $ 2 billion in support from the US government and other agencies.
“It looks like this vaccine is going to be relatively easy to make,” said virologist Angela Rasmussen of Columbia University. “Their downside is that similar protein subunit vaccines, for example the hepatitis B vaccine, take multiple injections to build immunity.”
In Britain, 15,000 volunteers (including Bingham) have been enrolled in phase 3 trials of the Novavax vaccine. The company says it hopes to get key data from this group in early 2021 and use it to get approval for the vaccine. Britain agreed to buy 60 million doses.
It remains to be seen how scientists receive these different vaccines. Trial results will be vigorously pursued and the controversy surrounding the Oxford-AstraZeneca vaccine will be repeated. A vaccine may sound good at preventing people from succumbing to serious illness, but how long could it provide protection? And how good will a vaccine be at preventing transmission of the virus and how well will it work in higher risk groups, such as the elderly? How easy will it be to manage and transport? It will take months, if not years, to answer all of these questions for each vaccine.
The good news for Britain is that it is very well positioned to make major contributions to solving these problems, said Jonathan Pearce, acting director of the Covid-19 response at the Medical Research Council. He added: “The UK has excellent medical data resources and an integrated healthcare system which has already enabled us to establish a world leading study to rate Covid-19 treatments. Our opportunity to contribute to the global good will be very high ”.