[ad_1]
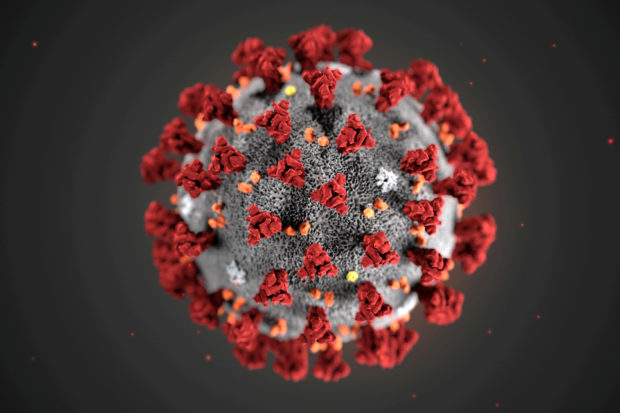
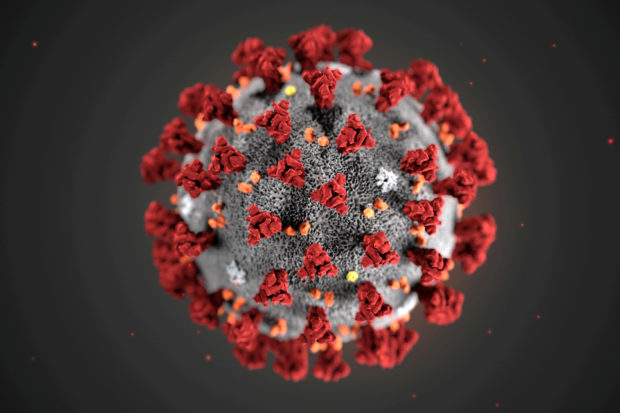
FILE PHOTO: The ultrastructural morphology exhibited by the 2019 novel coronavirus (2019-nCoV), which was identified as the cause of an outbreak of respiratory disease first detected in Wuhan, China, is seen in an illustration published by the Centers for Disease Control and Prevention (CDC) in Atlanta, Georgia, USA January 29, 2020. Alissa Eckert, MS; Dan Higgins, MAM / CDC / Prospectus via REUTERS.
People whose immune systems responded strongly to a measles, mumps and rubella (MMR) vaccine may be less likely to become seriously ill if infected with the new coronavirus, new data suggests.
The MMR II vaccine, manufactured by Merck and licensed in 1979, works by activating the immune system to produce antibodies.
Researchers reported in mBio on Friday that among 50 COVID-19 patients under the age of 42 who had received MMR II as children, the higher their titers – or levels – of the so-called IgG antibodies produced by the vaccine and directed against mumps. viruses in particular, the less severe are its symptoms.
People with the highest mumps antibody titers had asymptomatic COVID-19.
More research is needed to show that the vaccine prevents severe COVID-19. Still, the new findings “may explain why children have a much lower COVID-19 case rate than adults, as well as a much lower death rate,” co-author Jeffrey Gold, chairman, said in a statement. of the World Organization, in Watkinsville, Georgia. .
“Most children receive their first MMR vaccination around 12 to 15 months of age and a second between 4 and 6 years of age.”
Smoking increases cellular vulnerability to COVID-19
The UCLA researchers also found that exposure to cigarette smoke makes cells in the airways more vulnerable to infection by the new coronavirus.
They obtained cells that line the airways of five people without COVID-19 and exposed some of the cells to cigarette smoke in test tubes. They then exposed all the cells to the coronavirus.
Compared to cells not exposed to smoke, cells exposed to smoke were two or even three times more likely to be infected with the virus, the researchers reported Tuesday in Cell Stem Cell.
Analysis of individual cells in the airways showed that cigarette smoke reduced the immune response to the virus.
“If you think of the airways as the high walls that protect a castle, smoking cigarettes is like creating holes in these walls,” co-author Brigitte Gomperts told Reuters. “Smoking lowers natural defenses and this allows the virus to enter and take over cells.”
Cells infected with new coronavirus die
Cells infected with the new coronavirus die within a day or two, and researchers have found a way to see what the virus is doing to them.
By integrating multiple imaging techniques, they saw the virus create “virus copy factories” in cells that looked like clumps of balloons.
The virus also disrupts cellular systems responsible for secreting substances, the researchers reported Tuesday in Cell Host & Microbe.
In addition, it rearranges the “cytoskeleton,” which shapes cells and “serves as a rail system to allow the transport of various charges within the cell,” co-author Dr. Ralf Bartenschlager of the University of Heidelberg told Reuters, Germany.
When his team added drugs that affect the cytoskeleton, the virus had trouble making copies of itself, “which tells us that the virus needs to rearrange the cytoskeleton in order to replicate with high efficiency,” Bartenschlager said.
“We now have a much better idea of how SARS-CoV-2 changes the intracellular architecture of the infected cell and this will help us understand why cells die so quickly.”
The Zika virus causes similar cell changes, he said, so it might be possible to develop drugs for COVID-19 that also work against other viruses.
For more news on the new coronavirus, click here.
What you need to know about the coronavirus.
For more information on COVID-19, call the DOH hotline: (02) 86517800 local 1149/1150.
The Inquirer Foundation supports our healthcare leaders and still accepts cash donations to be deposited into the Banco de Oro (BDO) checking account # 007960018860 or donate through PayMaya using this link .
Read next
Subscribe to INQUIRER PLUS to get access to The Philippine Daily Inquirer and more than 70 other titles, share up to 5 gadgets, listen to the news, download from 4am and share articles on social media. Call 896 6000.
For comments, complaints or inquiries, please contact us.
[ad_2]

