
[ad_1]
“For the first time, our multidisciplinary team was faced with an ultrasound and an MRI of the fetus of a pregnant woman at 29 weeks’ gestation.
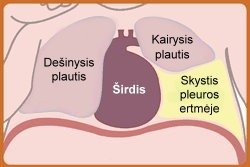
We saw that so much fluid was accumulating in the fetal chest that the heart was moving from left to right. After a while, the liquid began to accumulate on the right side as well. The situation was aggravated by the fact that due to the pathology of the fetus, the mother’s condition also began to deteriorate, ”says Prof. Prof. from the Center for Obstetrics and Gynecology. Diana Ramašauskaitė.

Diana Ramašauskaitė
Cases have been reported in the literature in which the accumulated fluids are drained while the fetus is still in the uterus because the mechanically pressed lung cannot develop normally. Unfortunately, in this case, the position of the fetus in the uterus was uncomfortable for such a procedure and the fetus was 32 weeks old, so the doctors made the decision to terminate the pregnancy and treat the newborn like a newborn.
“Fluid in the fetal chest can accumulate for various reasons: genetics, infection, various malformations. In this case, a bypass was detected in the left pleural cavity. After evaluating all the data, it was discovered that it was a lung sequestrant Pulmonary sequestration consists of lung tissue with separate blood flow, the blood is supplied directly from the aorta.
Because the abductor has no connection to the left lung tissue, it does not provide oxygen to the child’s body, so when the lung abductors are found, the children are operated on and the abductors are surgically removed. These surgeries are performed from 6 months of age ”, explains Dr., Head of the Department of Pediatric Surgery at Clinicas Santara. Arūnas Strumila.

Arūnas Strumila
© Photo from personal album
According to the pediatric surgeon, lung sequestrants do not usually cause any problems for the fetus, but in this case, fluid has begun to accumulate in the pleural cavity due to the torsion of the sequestrant. As the condition of the fetus deteriorated, the medical council decided to perform the EXIT procedure.
When is the EXIT procedure applied?
EXIT procedure Intrapartum treatment ex uterus) can help rescue a newborn in cases where the fetus is still poorly prognostic due to critical respiratory illness or birth defects. During pregnancy, oxygen from the placental fetus reaches the umbilical cord, so it is not necessary to use the lungs before birth. In a newborn and on the first inhalation, the lungs open and begin to function, the oxygen supply from the placenta becomes unnecessary, and the placenta quickly separates from the uterus.
EXIT procedūra
© Santara Clinic
“In rare cases, the fetus can develop congenital malformations that prevent it from breathing normally at birth. In such cases, the fetus feels fine before birth because the placenta performs lung function. But when a newborn is born and tries to inhale, cannot fill the lungs with air. If such a newborn becomes depressed and is cut immediately, the umbilical cord will not receive oxygen and will develop hypoxia (lack of oxygen). The EXIT procedure allows to compensate for this lack of oxygen and provides a few minutes of time precious for the first steps in the treatment of the newborn before he inhales for the first time ”, says Dr. Yelena Volochovich, Head of the Medical Competition at Fruit Centro de Clínicas Santara.
For this case, the doctors of the Santara clinics prepared with special responsibility: they anticipated possible complications, prepared for them, coordinated the activities of the individual teams. At one point, the operating room had 24 medical staff members: obstetricians, gynecologists, imaging specialists, anesthesiologists, a neonatal resuscitation team, and pediatric surgeons.

Clinicas Santara staff during the operation of Jelena Volochovich during the operation team
Gold for three and a half minutes
According to the head of the neonatal department of the Santara clinics dr. Ingrida Pilypienė, shortly after the baby was born, without squeezing or cutting the umbilical cord, the pediatric surgeons removed the fluid from the chest. The procedure took 3.5 minutes before the newborn still received oxygen through the mother’s umbilical cord. They were the golden minutes in which the medical team could do what was necessary and not worry about the newborn running out of air.
“The newborn resuscitation team had to resuscitate the newborn before it was separated from its mother. This case only reaffirmed that the Santara clinics have a multidisciplinary team that can provide assistance in complex and extremely rare cases. A good outcome depends on many things: accurate diagnosis of the pathology, monitoring of maternal and fetal conditions, planning and execution of the operation itself ”, says Prof. Diana Ramašauskaitė.
Neonatal resuscitation and intensive treatment after birth
“As expected, the newborn’s condition was very difficult at birth. The fluid accumulated in the pleural cavity had compressed the lungs, especially the left, pushing the heart and large blood vessels to an uncharacteristic place. While surgeons were trying to remove the fluid that had collected in the pleural cavity, a team of neonatologists began to resuscitate the newborn. A tube was inserted into the trachea, through which the newborn was given artificial respiration, and all the other steps necessary for resuscitation were taken, ”says the Associate Head of the Santara Clinics Neonatology Center. Arūnas Liubšys.

Dr. Arūnas Liubšys
After a successful resuscitation, cardiac function returned to normal and the newborn was transferred to the intensive care unit after stabilization. The neonate continued to be monitored and treated in collaboration with neonatologists, pediatric surgeons, pediatric cardiologists, pediatric radiologists, and other professionals. There was a gradual expansion of the lungs and an improvement in breathing, but it was immediately found that the patient had very high pressure in the blood vessels of the lungs, called pulmonary hypertension, which severely worsened blood oxygenation and heart function . Special artificial respiration had to be used: high-frequency oscillating ventilation, inhalation of nitric oxide, which dilates the blood vessels in the lungs, thus reducing the increase in pressure in them.
Neonatologist doctor doc. Dr. A. Liubšys states that regular infusions of drugs that promote heart function and vascular tone are not possible. Through the tube (drain) inserted into the pleural cavity, there was a constant separation of fluid that still accumulated, gradually diminishing. The newborn’s condition improves daily and the necessary treatment could be gradually reduced. Today, the newborn’s condition is stable and his life is no longer in danger. It is true that another operation is waiting for the baby – the removal of pulmonary sequestration, but it can be performed later, when the baby is a few months old and fully strengthened.
The director of the Neonatology Center was pleased that the professionalism, coordinated work and extraordinary efforts of the great medical team made it possible to save another small and delicate creature.
It is strictly prohibited to use the information published by DELFI on other websites, in the media or elsewhere, or to distribute our material in any way without consent, and if consent has been obtained, it is necessary to indicate DELFI as the source. .
[ad_2]