[ad_1]
WASHINGTON: Remdesivir has been shown to speed recovery times for Covid-19 patients in a major US-led trial. USA, becoming the first drug with proven benefit against the disease.
Here is what you need to know.
What is remdesivir?
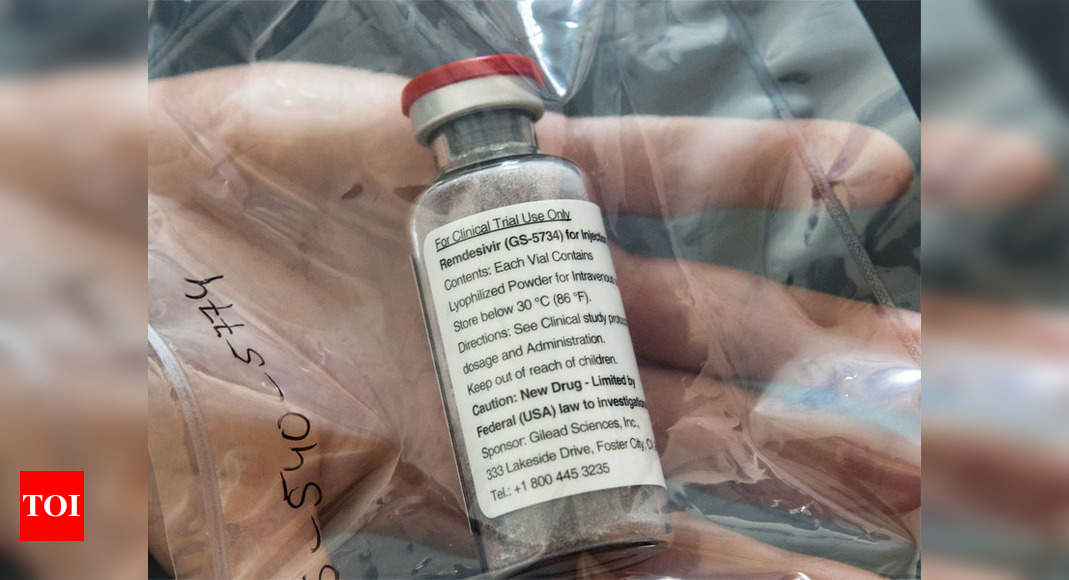
Remdesivir is a broad-spectrum experimental antiviral made by the American pharmacist Gilead Sciences that was first developed to treat Ebola, a viral hemorrhagic fever.
It showed promise in a primate study in 2016 and was then rolled out for a major trial in the Democratic Republic of the Congo, where it was compared to three other drugs.
That study ended in 2019 when it was discontinued because it did not increase survival rates as much as two monoclonal antibody drugs, which are laboratory-designed immune system proteins.
In February, the US National Institute of Allergy and Infectious Diseases. USA (NIAID) announced that it was dusting off remdesivir to investigate SARS-CoV-2, the pathogen that causes Covid-19, because it had shown promise in animal testing against other SARS and MERS coronaviruses.
Coronavirus block: latest updates
How effective is it?
NIAID announced the results of its trial involving more than 1,000 people on Wednesday, and found that hospitalized Covid-19 patients with respiratory distress improved faster than those who received a placebo.
Specifically, patients who took the drug had a 31 percent faster recovery time.
“Although the results were clearly positive from a statistically significant point of view, they were modest,” Anthony Fauci, the scientist who heads NIAID, said Thursday.
In other words, while it works, it is not a miracle cure.
However, it is considered a “proof of concept” that could pave the way for better treatments, just as the first drugs developed to treat HIV in the 1980s were not as effective as those used today.
The results suggested that remdesivir could reduce mortality rates from 11.7 percent to 8.0 percent, but these data are considered less reliable because they were above the limit of statistical significance.
Why have there been mixed results?
Findings from the US-led trial. USA They were announced the same day that the results of a smaller study were published in The Lancet, which found no statistical benefit from remdesivir.
Just over 200 people in Wuhan, China participated in this study, and it was also a randomized controlled trial, considered the gold standard for evaluating treatments.
However, it is important to note that he had to stop early because he was unable to recruit enough patients and was approximately five times smaller than the NIAID study.
“The numbers in the trial are too small to draw firm conclusions,” said Stephen Evans, medical statistics expert at the London School of Hygiene & Tropical Medicine.
When could it be available?
Remdesivir has already been administered to patients around the world, both in clinical trials and abroad, with Gilead responding to “compassionate use requests” for emergency access.
In the United States, the Food and Drug Administration (FDA) is expected to soon issue an “emergency use authorization” that would further expand its use, before formal approval.
“I was talking to the FDA commissioner yesterday afternoon, last night, and he’s moving very fast,” Fauci said Thursday.
“They haven’t made a final decision yet, they haven’t announced it, but I would project that we’ll see it reasonably soon.”
Since the drug is complex to manufacture and is given by injection, rather than a pill, there have been questions about whether the supply might be limited initially.
In an open letter released Wednesday night, Daniel O’Day, the president of Gilead, wrote that the company currently had 1.5 million doses completed or nearly completed.
“We had estimated that this would be 140,000 treatment courses based on a treatment duration of 10 days,” he said, but another trial has shown that five-day courses are as effective as ten.
This means that “we can significantly increase the number of courses available, all of which Gilead has promised to donate,” O’Day said.
The company is also looking to potentially develop an inhaled formulation, but has not provided a timeline.
How does it work?
Remdesivir belongs to a class of drugs that directly attack viruses.
It is what is called a “nucleotide analog” that mimics adenosine, one of the four basic components of RNA and DNA.
“The virus is not very careful about what it incorporates,” said virologist Benjamin Neuman of Texas A&M University.
“Viruses generally try to go fast and change speed as a precaution.”
Remdesivir is stealthily incorporated into the virus genome instead of adenosine, which in turn cuts off the replication process.
[ad_2]
Here is what you need to know.
What is remdesivir?
Remdesivir is a broad-spectrum experimental antiviral made by the American pharmacist Gilead Sciences that was first developed to treat Ebola, a viral hemorrhagic fever.
It showed promise in a primate study in 2016 and was then rolled out for a major trial in the Democratic Republic of the Congo, where it was compared to three other drugs.
That study ended in 2019 when it was discontinued because it did not increase survival rates as much as two monoclonal antibody drugs, which are laboratory-designed immune system proteins.
In February, the US National Institute of Allergy and Infectious Diseases. USA (NIAID) announced that it was dusting off remdesivir to investigate SARS-CoV-2, the pathogen that causes Covid-19, because it had shown promise in animal testing against other SARS and MERS coronaviruses.
Coronavirus block: latest updates
How effective is it?
NIAID announced the results of its trial involving more than 1,000 people on Wednesday, and found that hospitalized Covid-19 patients with respiratory distress improved faster than those who received a placebo.
Specifically, patients who took the drug had a 31 percent faster recovery time.
“Although the results were clearly positive from a statistically significant point of view, they were modest,” Anthony Fauci, the scientist who heads NIAID, said Thursday.
In other words, while it works, it is not a miracle cure.
However, it is considered a “proof of concept” that could pave the way for better treatments, just as the first drugs developed to treat HIV in the 1980s were not as effective as those used today.
The results suggested that remdesivir could reduce mortality rates from 11.7 percent to 8.0 percent, but these data are considered less reliable because they were above the limit of statistical significance.
Why have there been mixed results?
Findings from the US-led trial. USA They were announced the same day that the results of a smaller study were published in The Lancet, which found no statistical benefit from remdesivir.
Just over 200 people in Wuhan, China participated in this study, and it was also a randomized controlled trial, considered the gold standard for evaluating treatments.
However, it is important to note that he had to stop early because he was unable to recruit enough patients and was approximately five times smaller than the NIAID study.
“The numbers in the trial are too small to draw firm conclusions,” said Stephen Evans, medical statistics expert at the London School of Hygiene & Tropical Medicine.
When could it be available?
Remdesivir has already been administered to patients around the world, both in clinical trials and abroad, with Gilead responding to “compassionate use requests” for emergency access.
In the United States, the Food and Drug Administration (FDA) is expected to soon issue an “emergency use authorization” that would further expand its use, before formal approval.
“I was talking to the FDA commissioner yesterday afternoon, last night, and he’s moving very fast,” Fauci said Thursday.
“They haven’t made a final decision yet, they haven’t announced it, but I would project that we’ll see it reasonably soon.”
Since the drug is complex to manufacture and is given by injection, rather than a pill, there have been questions about whether the supply might be limited initially.
In an open letter released Wednesday night, Daniel O’Day, the president of Gilead, wrote that the company currently had 1.5 million doses completed or nearly completed.
“We had estimated that this would be 140,000 treatment courses based on a treatment duration of 10 days,” he said, but another trial has shown that five-day courses are as effective as ten.
This means that “we can significantly increase the number of courses available, all of which Gilead has promised to donate,” O’Day said.
The company is also looking to potentially develop an inhaled formulation, but has not provided a timeline.
How does it work?
Remdesivir belongs to a class of drugs that directly attack viruses.
It is what is called a “nucleotide analog” that mimics adenosine, one of the four basic components of RNA and DNA.
“The virus is not very careful about what it incorporates,” said virologist Benjamin Neuman of Texas A&M University.
“Viruses generally try to go fast and change speed as a precaution.”
Remdesivir is stealthily incorporated into the virus genome instead of adenosine, which in turn cuts off the replication process.