
[ad_1]
The herd immunity strategy, which would allow the majority of the population to gain resistance to the virus by becoming infected and then recover, could lead to less economic devastation and human suffering than restrictive blocks designed to stop the virus from spreading, according to several experts. began to argue in the nation of 1.3 billion people.
Blog: Level The Field: News Producers Can’t Keep On Costing As Digital Platforms Deplete Profits
“No country can afford a long period of confinement, much less a country like India,” said Jayaprakash Muliyil, a leading Indian epidemiologist. “You may be able to reach a point of collective immunity without the infection actually reaching the elderly. And when the collective immunity reaches a sufficient number, the outbreak will stop and the elderly will also be safe.”
A team of researchers from Princeton University and the Center for Disease Dynamics, Economics and Policy, a public health advocacy group based in New Delhi and Washington, have identified India as a place where this strategy could succeed because its disproportionately young population would face less risk of hospitalization and death.
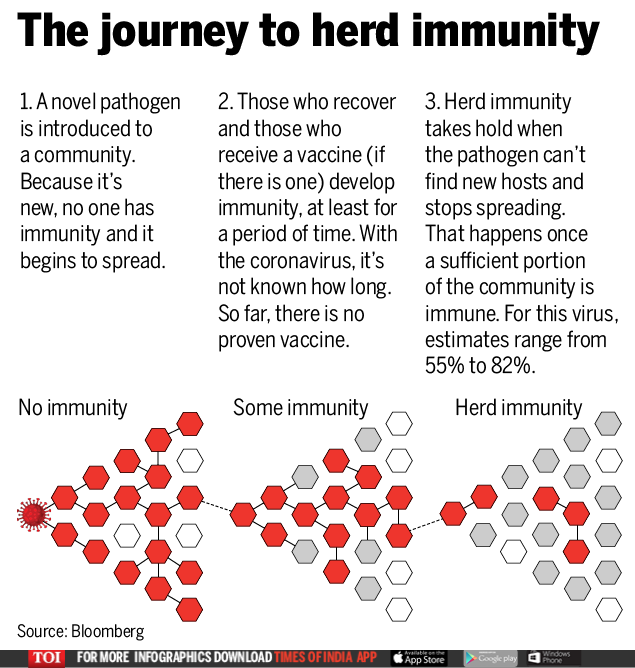
They said allowing the virus to unleash in a controlled way over the next seven months would grant immunity to 60% of the country’s population in November and thus stop the disease.
Read our coronavirus blog live for the latest news and updates
Mortality could be limited as the virus spreads compared to European nations like Italy, given that 93.5% of the Indian population is under the age of 65, they said, although no projections of deaths were published.
The radical proposal underscores the challenges facing the poorest developing countries, including nations like Indonesia and some in sub-Saharan Africa, to stem the epidemic using the closure measures that have been taken by advanced economies.
The impossibility of social distancing in crowded living conditions, as in many cities and towns in India, the lack of test kits to detect infections and the human suffering that occurs in confinements suggests that a different path may be necessary in these places .
More in COVID-19
To do this, the Princeton and CDDEP team recommends lifting the strict India shutdown, which extended until May 3, and allowing the majority of the population under the age of 60 to return to normal life, although it would still be encouraged social distancing, masks would be required and large gatherings would be prohibited. The reopening would be accompanied by an effort to evaluate as many people as possible and isolate confirmed and suspected cases.
Prime Minister Narendra Modi’s government has given no indication that it plans to adopt such a strategy.
However, the government has established criteria that effectively ration the coronavirus tests, limiting them to the very sick or at higher risk. Critics who suspect that the disease has spread much more than official figures suggest say the government’s restrictive criteria amount to allowing the disease to spread.
“In a sense, you say we will allow them to become infected and recover, and we will care only for those who are sick,” said T Sundararaman, the New Delhi-based global coordinator of the People’s Health Movement, a public health group. . “That’s the policy, that’s what it amounts to.”
The government has maintained that its test criteria give an accurate count of the number of cases in India and says that the disease is not spreading without monitoring in the community. However, as India has increased the evidence, it is finding more cases every day, bringing the national count to 19,984, with 640 deaths, as of April 22.
But if questions remain about the extent and severity of the India outbreak, the costs of the government shutdown are clear. Local governments have had to set up camps to house 1.25 million migrants who left the cities when they lost their jobs, while food camps feed 7.5 million daily wage earners who were also left destitute by the closure. . There are already indications that these provisional measures are beginning to weaken.
“We are dealing with compensation against hunger, hunger, all these other things,” said Ramanan Laxminarayan, CDDEP director and Princeton researcher. By allowing the coronavirus to spread in a controlled way, “there will undoubtedly be deaths, but it will be much smaller this way, and it will open us up for business by November,” he said.
But the strategy has already been controversial internationally. The UK adopted and then abandoned it early in the pandemic after projections showed that its healthcare system would be overwhelmed by the resulting hospitalizations. That short delay is still blamed for the slow response by the British government in testing the virus.
Risky strategy
Even in a country like India with a young population, the concept has inherent risks. Allowing people to become infected will inevitably bring many more patients to hospitals. The researchers say India will urgently need to expand critical care and isolation bed capacity to ensure multiple waves of patients do not become victims before herd immunity is achieved.
Another risk is that India’s worst air pollution and high rates of hypertension and diabetes have compromised young people’s health, which means that mortality from the virus could be higher than expected. People can disappoint their guards and not follow the guidelines of social distancing.
“I would be concerned if it alleviates the concerns of younger people, who are still at substantial risk,” Jason Andrews, an assistant professor of medicine at Stanford University, said in an email. “The message in particular may make younger people perceive themselves as less risky than themselves and not understand their potential role in transmission.”
And since the new coronavirus only debuted in humans sometime late last year, there are still many things that are unknown. Virus immunity may be a more complex process than expected. A group of researchers estimated that up to 82% of the population would have to become infected before immunity from the herd could be achieved.
“My opinion is that there are several questions about whether it can work,” said Marc Lipsitch, professor of epidemiology at the TH Chan School of Public Health at Harvard University. “The main questions are how much immunity do we need in the population and how much immunity does each person get as a result of infection.”
Then there is also the question of whether it is possible to isolate the highest-risk portion of the population in densely populated India, where several generations commonly live under one roof.
Ultimately, researchers pushing for the strategy argue that cultivating herd immunity may be the best of several bad options.
“I think eventually all countries will follow this Indian model,” said Laxminarayan. “Because otherwise, we’re going to be locked up all the time until June of next year.”