Updated: August 29, 2020 9:25:28 am
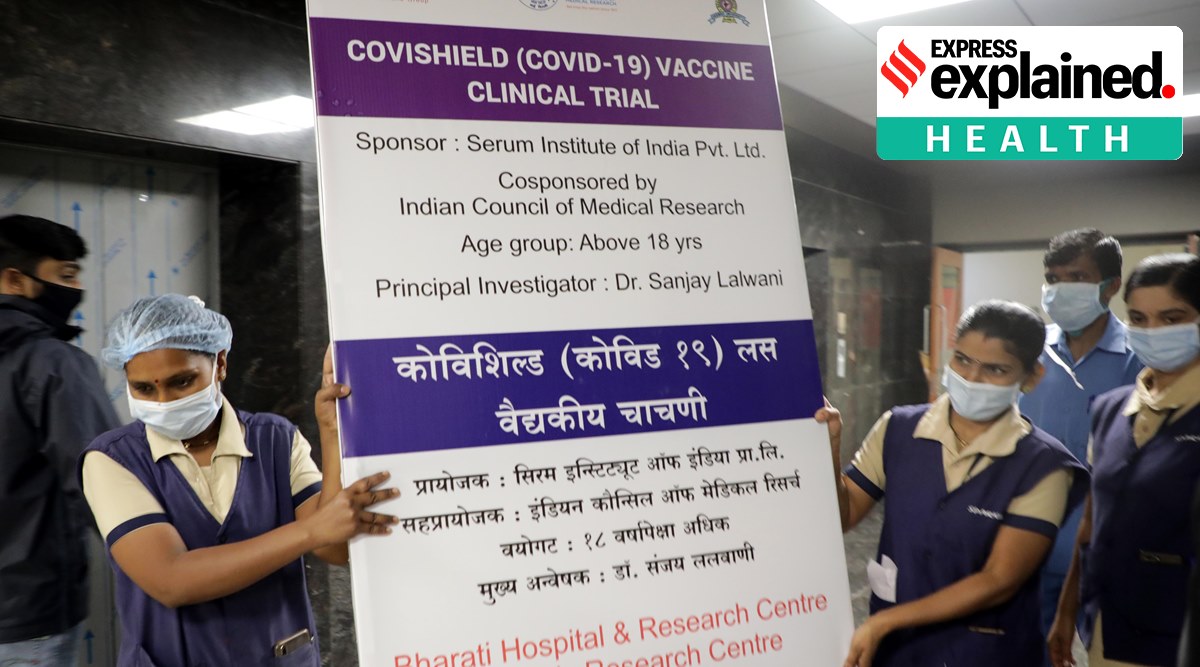
 Oxford-AstraZeneca vaccine trials begin in Pune on Wednesday. (Express photo: Arul Horizon)
Oxford-AstraZeneca vaccine trials begin in Pune on Wednesday. (Express photo: Arul Horizon)
The United States has entered into multi-million dollar deals with at least six major pharmaceutical companies to ensure the supply of a combination of 800 million doses of vaccines they are developing separately for the new coronavirus. That’s more than two doses for every American citizen. The agreements mean that if any of these companies are successful in developing a vaccine, they would be obligated to provide the agreed-upon supplies to the United States before anyone else.
The UK has similar agreements with a number of companies to ensure 340 million doses, or about five doses per capita. The European Union and some other countries like Mexico have also reached similar agreements. Read in Tamil
A new vaccine against the coronavirus is still some distance away, if we rule out vaccines developed by Russia and China for which the international demand is not very well evaluated. But the way countries pre-book vaccine supplies, often dumping billions of dollars in candidate vaccines whose success as of now is uncertain, has raised questions about the accessibility and affordability of a vaccine, provided that ultimately To develop. Also has gave rise to a term called “vaccine nationalism”.
Why is “vaccine nationalism” a cause for concern?
Concerns arise from the fact that these advance deals are likely to make the vaccine inaccessible to large parts of the world that don’t have the money to bet on candidates whose success is not guaranteed.
After all, there is a limited capacity to produce a vaccine. The wait for a vaccine for these countries could be prolonged because what is produced in the first months or years would have to be sent to the richest countries to meet contractual obligations.
Also, not all candidate vaccines are likely to be successful. Those that do would be in high demand, especially from countries that have entered into advance agreements that have clauses to allow for increased supply for more money. Thus, it would drive up the prices of the vaccine, making it potentially unaffordable for a large number of countries.
An ideal situation would be to ensure that vaccines are first made available to those who need them most. Experts agree that front-line healthcare workers, those in emergency duty, the elderly and the sick, pregnant women and other equally vulnerable populations around the world must first have access to vaccines. But that is not what seems to be happening.
Also in Explained | Who will get the first Covid-19 vaccine in India and other countries?
Why do countries accumulate vaccines?
The coronavirus vaccine is being used by governments around the world as an opportunity to impress their own people, as well as the international community. To their citizens, governments want to show how concerned they are about their safety and health, for which they want to stockpile as many vaccines as they can. And for the international community, and also for their own audience, they want to show off their scientific ability and expertise. This is also why China and Russia have approved vaccines that have not yet completed the necessary trials to show that they are safe and effective. There are political dividends for declaring yourself the first to develop a vaccine.
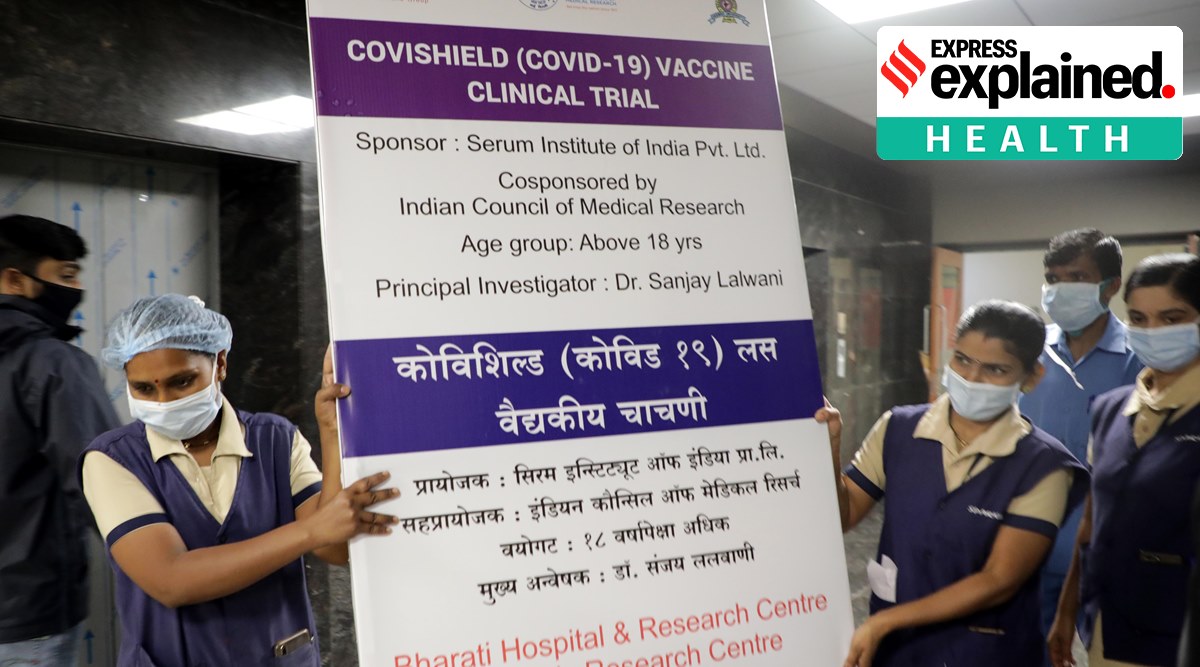
 Covishield, the Oxford-AstraZeneca vaccine candidate, is administered to a volunteer in Pune. (Express photo: Arul Horizon)
Covishield, the Oxford-AstraZeneca vaccine candidate, is administered to a volunteer in Pune. (Express photo: Arul Horizon)
Are there precedents for such a prior reservation in other outbreaks?
Indeed, fears about the shortage and unaffordability of the new coronavirus vaccine are not unfounded. There have been precedents: in 2009, after an outbreak of H1N1 influenza, or swine flu, rich countries had accumulated vaccines in a similar way to the previous reserve that is happening now. As a result, many countries in Africa did not have access to these vaccines for months. The United States and some European countries eventually agreed to deliver 10% of their stocks to other countries, but only after it became clear that they no longer needed the vaccines for themselves.
Similarly, antiretroviral drugs to treat HIV patients were unavailable in Africa, the worst-affected region, for several years after their development in the 1990s.
Scientists and experts have argued that such a strategy might not work very well even for countries that can stock up on vaccines. If some parts of the world continue to suffer from the epidemic due to lack of access to the vaccine, the virus will remain in circulation for much longer than it would have otherwise. That would mean that other countries would remain at risk as well, at least economically, due to continued disruptions in global supply chains due to movement, labor and trade restrictions in large parts of the world.

So what is the way forward to tackle this problem?
It is not that there is no alternative path to this “me first” approach that richer countries have been adopting. The World Health Organization (WHO), along with some other international alliances, has launched a platform called the ACT (or Access to Covid19 Tools) Accelerator Program. Its goal is to accelerate the development, production and equitable access to Covid-19 vaccines, as well as therapeutics and drugs. The vaccine part of the program is called COVAX installation.
COVAX is supposed to do for the world what the richest countries are doing individually: invest money in the main candidate vaccines to accelerate their development and production. But it also has another important goal: to ensure that successful vaccines are equally accessible to all, at an affordable price. It seeks to achieve this by ensuring that all participating countries receive supplies to cover at least 20% of their population, at a uniform price. Then, as more doses of vaccine become available, they will be distributed to countries in proportion to the size of their populations and the extent of the problem they face.
Like the US and other countries that are entering into advance agreements, COVAX is supposed to fund research and development for multiple candidate vaccines. As of now, the facility endorses nine prominent candidates. Countries are asked to join the platform and contribute funds, so that everyone can benefit. But although more than 170 countries are in talks, very few of them have agreed to fund the initiative. Recently, the WHO noted that while it needed at least $ 100 billion for the COVAX installation, so far not even 10% of the amount had been raised.

For the latest news explained, download the Indian Express app.
© The Indian Express (P) Ltd
.