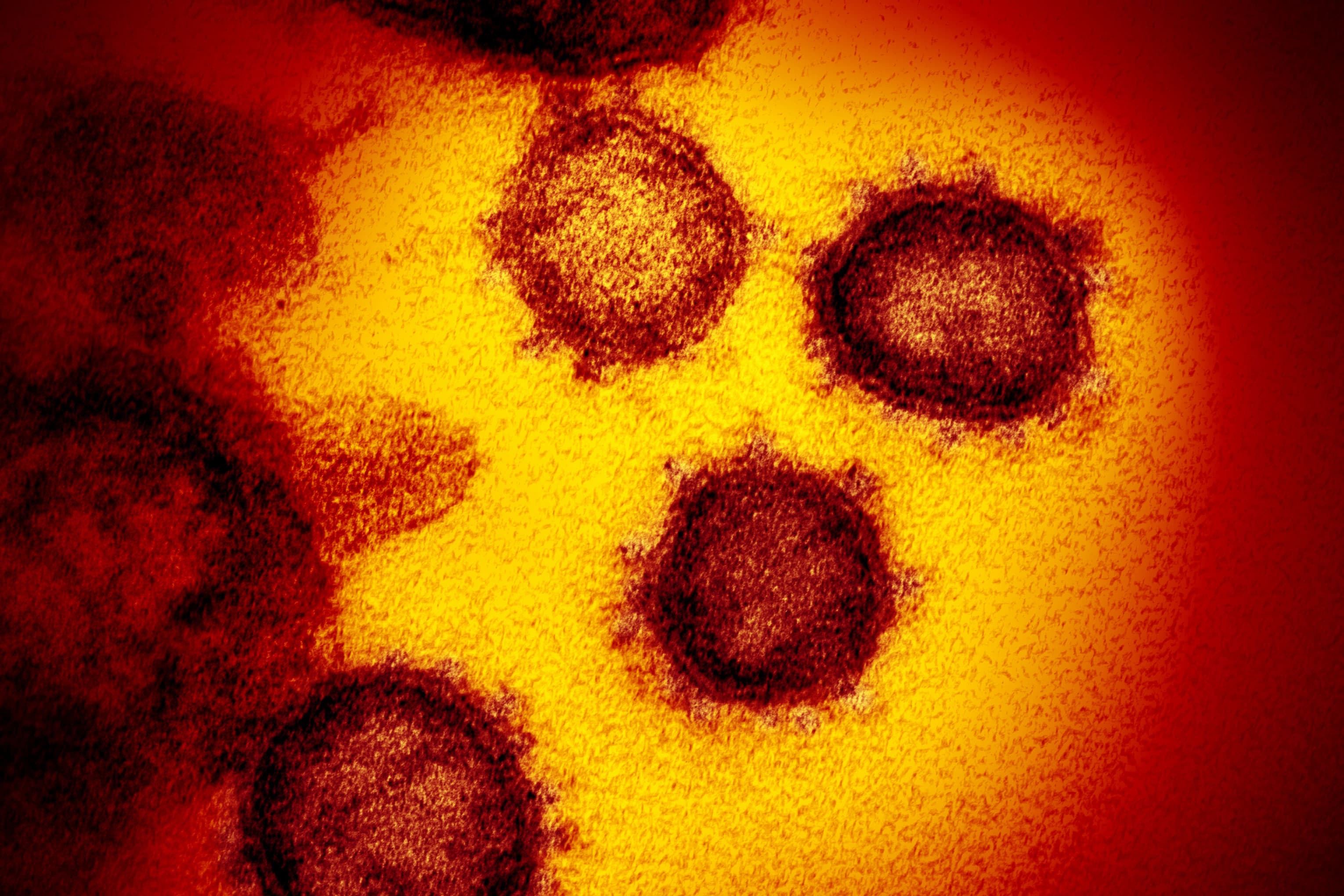
This transmission shows the electron microscope image SARS-CoV-2, also known as 2019-nCoV, the virus that causes COVID-19. U.S. No different from the patient, emerging from the surface of cultured cells in the laboratory.
Source: NIAID-RML
Although the global Covid-19 infection is declining worldwide, leading U.S. health officials are warning of infection, with newer, more infectious – and possibly more – deadly strains of the virus appearing in the U.S.
Scientists are not surprised by the emergence of new variants and have reiterated that currently available vaccines should still work against them – albeit, slightly less effective than the original, “wild” strain. However, the U.S. Top officials and infectious disease experts are concerned that these highly contagious forms, especially B1.rain..7 strain, are emerging in the UK. May reverse the current following route of infection and delay recovery from the country’s epidemic. .
“I think we should assume that the next wave of case growth, to the extent that we have there, will be with B.1.1.7, and that’s something I think everyone should be more careful about,” White said. Andy Slavit, senior adviser to the House’s Covid-19, told MSNBC last week. “Glad to see the number of cases declining, but it can be misleading.”
Why viruses change
As the coronavirus spreads, it makes a large number of copies of itself, and each version is slightly different than before, experts say. SARS-COVI-2, the virus that causes COVID-19, has ample opportunities to spread and replicate. As more people become infected, the likelihood of problematic changes increases.
U.S. The three main “types of concern” with officers were first identified in the United Kingdom, South Africa and Brazil. The B1.1.7 variant, first found in the UK, is multiplying rapidly in the United States and is expected to become the country’s dominant strain by March, according to the U.S. Department of Disease Control and Prevention. According to a January study by the Centers.
By mutation, the virus is simply trying to “go to the next host and make itself more,” said Dr. Borber, an infectious disease specialist at the University of Michigan in Ann Arbor. Adam Luring Ring told the JAMA network in a Feb. 4 interview. . Like other coronaviruses, SARS-CoV-2 mutates more slowly than other viruses. Flu is like that because it has a “proofreading” enzyme that fixes some changes when it mimics.
In other cases, “escape mutation” allows the virus to adapt to “selective pressure”, which occurs when the virus is already infected, vaccinated, or treated with antibody therapy by a population already immune to it. Limits its ability to spread but does not prevent it.
“You might want to try new solutions about it,” Lauring said. “Either change will make you a better virus or a worse virus, and then you have the choice. For a better term, to survive the most appropriate way.”
Research shows that more worrying virus mutations may come from people who have an immune system because it takes longer for the body to respond and clear the virus, giving us more time to detect and change, said Dr. Scripps Research Institute President Dr. . Said Dennis Burton. Immunology and microbiology.
“If someone has the virus, and it clears up in a few days, you don’t have much of a chance to make a difference,” Burton told CNBC in a phone interview. “But if a person has a virus like the immunocompromised person, and they use the virus for weeks, they will have a much better chance of changing.”
Why some are worse than others
Infectious disease experts say that only a small number of different types cause public health concerns. Those types are usually easier to spread, cause more serious illness in infected people, or avoid some protection from vaccines and antibodies.
CDC Director Dr Rochelle Valensky told JAMA on Wednesday that the B1.1..7 variant is thought to be about 0% more transmissible and preliminary data suggest it could be 50% more viral or fatal.
There is also evidence that people infected with previous strains of the virus may be re-infected with the B1.351 version found in South Africa, said Vale Lansky, the White House’s chief medical adviser. Anthony Foki and Dr. Wrote in JAMA’s view with Henry Walkey, CDC’s Kovid event manager.
According to the CRC, SARS-Cavi-2 is a coronavirus, a large family of viruses known as “for crown-like spikes on their surface”. Researchers observe those spikes or S-proteins for mutation because they can bind the virus to cells or increase the amount of virus a person sheds.
The S-protein, called the “receptor binding domain,” acts like a “spike’s hand” that captures an object called the ACE2 receptor on human cells, said Dr. Daniel Griffin, told CNBC.
Griffin said mutations in S-proteins can be a problem because they are aimed at inactivating spikes antibodies that fight covid-19 and are created by natural infection or vaccination, Griffin said. They can also affect the effectiveness of monoclonal antibody therapies that prevent people from getting serious illness.
For example, the U.K. There are many different variations in the first identified B.1.1..7 variant, according to the CDC. One of the key mutations, N501Y, is a change in the spike protein that scientists believe helps the virus build up in cells.
The same key N 501 Y transformation has developed separately in the B.1.351 identified in South Africa and the P1 variant in Brazil. Both species have also developed another in relation to mutations in their spike proteins, known as E484K.
The CDC warns that this mutation, now identified in some B.1.1.7 cases, may be resistant to antibody drug therapy, and preliminary studies show that it may reduce the effectiveness of some vaccines.
“This is what really worries me,” Griffin told CNBC, referring to the E484K transformation.
What do these vaccines mean?
While the vaccine has yet to prove effective against variables, there are concerns that the B.1.351 strain may present some challenges.
In late January, large clinical trials from Johnson and Johnson and Novavax reported a decrease in their vaccines. Effectiveness when tested in South Africa, where the variable first came out. Novavax said his vaccine In South Africa, only 49% of the 44 Covid-19 cases were effective, and J&J said the vaccine was 57% effective in preventing the pathological Covid-19.
Kate O’Brien, the World Health Organization’s director of immunization, said on Thursday that the results did not provide much certainty because of the low number of test weapon cases in South Africa.
“We’re still in these early days of interpreting the evidence and, most importantly, getting more information about what’s really going on in terms of the disease,” O’Brien said in a press briefing. “In general, we see that vaccines maintain efficacy against the disease, however, at lower levels in settings, without variants, which is extremely prevalent.”
Pfizer and Modern
Clinical trials of Pfizer-Bioentech and Modern were performed before variants emerged, so scientists are conducting laboratory tests to determine how blood samples from people who have been vaccinated can be used to differentiate between different types of lab-built viruses. Reacts.
That study, which neutralized the virus from the sera in the blood and prevented it from recurring, showed a decrease in performance when tested against the B.1.351 variable. “It has been suggested (s) that currently used vaccines may be less effective in preventing infection due to this type,” W. W. Lensky, Fawski and W. Lk wrote from their point of view.
However, your body’s ability to fight the virus depends more than just neutralizing antibodies, including T cells and B cells, which can help fight the virus, but is not measured in initial lab assessments, Lauring said.
The good news is that the Pfizer and Moderna vaccines have shown such high efficacy rates in previous tests – about 95%. Experts say, there is a cushion that will bring a dip in their performance while still considered effective by doctors. Shots have also been shown to provide protection against contractions of severe forms of the disease that can result in hospitalization or death.
Both Pfizer and Moderna have already said they are working on a booster shot for their vaccines that will hold better against the B1.351 strain.
Looking for change
The variant B.1.1.7 was first identified in the United Kingdom in December, but is thought to have emerged at some point in September. Many experts have credited the UK’s ability to do extensive genomic sequencing to find variables.
Genomic sequencing is a laboratory technique that breaks down the genetic code of a virus, allowing researchers to observe how it changes over time and understand how these changes can affect it, according to the CDC.
U.S. In, now the CDC. According to the latest figures, 1,661-documented Covid-1 cases with BH1..7 variant, 22 cases with B-1.551 variant and P. Officials acknowledge that U.S. Indexing a small portion of the case, and spreading the variables as wide as possible. However, the federal government has recently tried to create a sequence of how many samples per week to detect these types and other changes that can make a local change.
The CDC has partnered with public health and commercial laboratories to quickly scale the country’s genomic sequencing. Vale Lansky told Jaman on Wednesday that in January, U.S. It was sequencing only 250 samples per week, which has since increased to “for thousands of people.” “We are not where we need to be,” she added.
Dr. Ilham Mesoudi, director of the University of California at Irvine Center for Virus Research, said the process can be time-consuming and labor intensive, but the emerging strain will be missed if laboratories do not index a certain percentage of all positive covids. 19 test results to detect new mutations, he said.
“Now we’re trying to catch up,” Mesaudi said in a phone interview with CNBC. “We are, ‘Let’s go back and see if we have this.'”
Mask, social distance
Rapidly spreading variables through hygienic measures such as wearing masks, social distance and hand hygiene renew the importance of suppressing coronavirus, such as buying time to prevent further change and giving the country life-saving vaccines.
But coronavirus variants are not the only problem for the United States. The head of the CDC warned on Wednesday that if the virus spreads to other parts of the world that are inadvisable, it could lead to a change that could threaten vaccines widely deployed in other countries.
Eventually, the whole world will need to build immunity to the virus, otherwise the variables will remain a problem, Burt told CNBC.
“Sooner or later variables will be found everywhere if they have a big advantage.” Said Burt. “It’s a global problem, it’s not just a problem of any one country.”
.