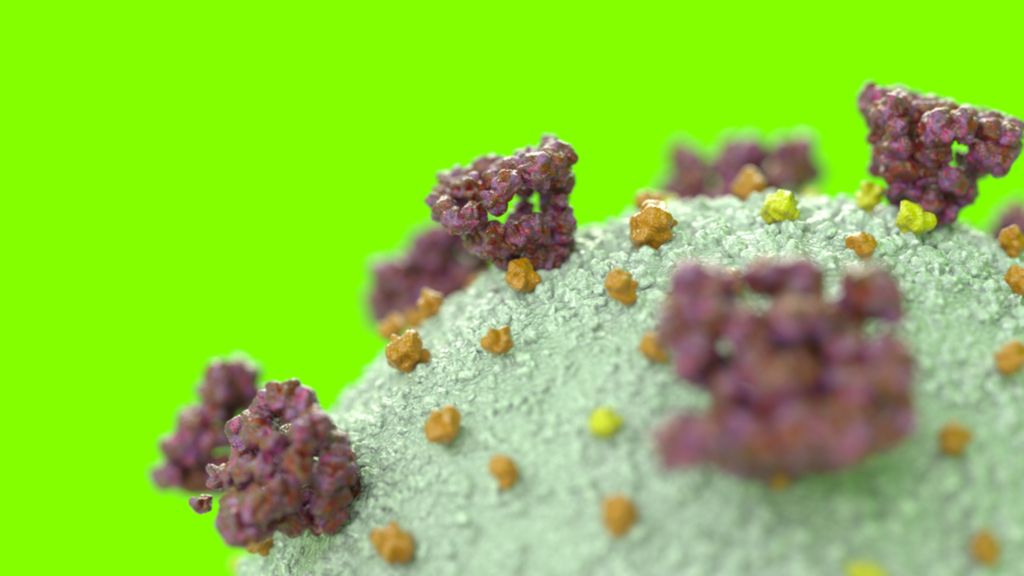
The coronavirus that causes COVID-19 infects cells by plugging in a receptor on their surface. Now, by making a “decoy” of that receptor, scientists are aiming to track the virus’ attack.
In a new study, published August 4 in the journal Science, researchers designed such a decoy and found that the coronavirus bound tightly to the imposter receptor, and once applied, the virus could not infect primates in a laboratory. The decoy bound to the virus as tightly as a neutralization antibody, a Y-shaped molecule generated by the immune system to catch the virus and prevent cells from infecting.
Neutralizing antibodies are the “best thing that makes the human body … so that’s our goal” – to have a decoy receptor that just as cleverly attaches to the coronavirus, studies author Erik Procko, an assistant professor of biochemistry University of Illinois at Urbana Campaign, told Live Science. The team found that their newly designed decoy, known as sACE2.v2.4, tightly binds both the novel coronavirus and SARS-CoV, a related virus that caused outbreaks of severe acute respiratory syndrome in the early 2000s.
Related: 14 myths of coronavirus busted by science
If the decoy works in animals as it does in cell culture, it could be developed into a COVID-19 treatment and preventive therapy for humans. That said, the research is still in very young stages and no decoy receptor has ever been approved as a treatment for an infectious disease, Procko said.
“This would be something new, if successful,” because it would be the first lockdown, approved as an antiviral, he said.
Design of a decoy
Some decoy receptors have been approved by the US Food and Drug Administration (FDA) for the treatment of diseases involving inflammatory and immune systems, such as the rare “familial cold autoinflammatory syndrome” which causes recurrent fever, joint pain and inflammation of the eyes, according to a 2013 report in the journal Frontiers in Immunology. However, decoy receptors developed as antiviral treatments have historically hit roadblocks on their way to approval.
The first decoy designed to control a virus mimics a natural receptor found on immune cells called CD4, which binds to HIV, according to a 2008 report in the journal Current opinion in biotechnology. While promising in studies using lab-grown HIV strains, CD4 decoys did not bind effectively to strains isolated from HIV / AIDS patients, according to the report. To date, no CD4 decoys have been graduated from clinical trials and are approved for use in patients. The same goes for the decoys designed to treat rhinovirus, foot and mouth disease virus, hepatitis A and SARS-CoV.
Procko notes that in order to be a successful antiviral, a decoy receptor must meet two important criteria:
First, it should not disrupt important bodily functions, given that natural receptors often play multiple roles in the body. For example, the ACE2 receptor, which exploits COVID-19 as a gateway to cells, also helps control blood volume and lower blood pressure, he said. By infecting cells with ACE2 receptors, COVID-19 actually interferes with ACE2 activity in the body – a decoy ACE2 receptor could potentially “rescue” some of this lost activity by leaving natural receptors open for business, instead of bound to it coronavirus, said Procko.
Related: 20 of the worst epidemics and pandemics in history
However, decoy ACE2 receptors could cause unexpected side effects, so researchers should check for these in animal studies and early clinical trials, he added.
In addition to being safely managed, a decoy receptor must show high affinity for the virus that is targeted, which means that it is tightly bound to the virus in human cells.
“To be a good binder, with high affinity, you have to bind your target quickly and you have to slowly get away from your target,” Procko said. To find a cure that binds well to SARS-CoV-2, Procko and his colleagues eliminated thousands of inadequate ACE2 copycates using an experimental technique known as “deep mutagenesis.”
So what is deep mutagenesis? Think of a Vegas slot machine – a mix of three different fruits equals a certain payout (if not). DNA is the same: a set of three letters code for a single amino acid, as a protein building block. In this case, the team shuffled the three-letter segments into 117 spots in human DNA that past studies suggested affect how tightly coronavirus bound to the ACE2 receptor. This allowed the researchers to essentially pull over “the slot machine lever” completely to study how the exchange of each amino acid (one spin of the slot machine) for another affected the coronavirus binding of ACE2 receptor. In this case, the scrubbed DNA was expressed in different versions of human cells in a laboratory.
“You can exhaustively test many, many thousands of mutations to see which ones are relevant,” Procko said.
After producing cells with mutant ACE2 receptors – socks based on twisted DNA segments, the researchers exposed the cells to the part of SARS-CoV-2 that is locked up in the ACE2 receptor, known as the receptor binding domain. They found that sACE2.v2.4 shows the highest affinity for the virus; the researchers then developed a version of the decoy that can exist in the body without attaching to a cell, because the loose receptor is all that would be needed for a future medicine.
The following steps
Compared to an unmodified ACE2 receptor, “less than 1% of the entire protein sequence has been altered” to make the key, Proko noted. If fully developed as a treatment for humans, the decoy receptor would likely be delivered into the body by an injection or as a mist inhale, he said. Drugs derived from living things, such as the decoy receptor, are “often long-lived,” and can last a week or more in the body, he said.
A decoy receptor would serve a similar purpose antibody cocktails designed to treat COVID-19, which would contain multiple antibodies that bind to SARS-CoV-2 in different ways. However, a report published June 15 in the magazine Science suggests that the virus can mutate to escape the grip of specific antibodies – a decoy receptor may be reliable in the long run because the virus will be less likely to mutate in such a way that it no longer binds to ACE2, said Procko. The fact that sACE2.v2.4 binds both SARS-CoV-2 and its predecessor SARS-CoV tightly supports this idea, given that both viruses use ACE2 to break down cells.
Procko founded a start-up called Orthogonal Biologics to work on the ACE2 decoy earlier this year, along with study author Kui Chan, who serves as Chief Operating Officer. The next step is to do animal studies, and as the treatment progresses to human studies, they should show that the decoy can be reliably produced on large scales.
Interestingly, anACE2-decoy, which was developed by researchers linked to Apeiron Biologics, is already being tested in clinical trials for the treatment of COVID-19, and so far it appears safe in both healthy people and those with lung disease, according to a statement of the company. The major difference is that the existing decoy closely resembles the native ACE2 receptor, and is not mutated to bind as tightly as possible to SARS-CoV-2, whereas sACE2.v2.4 does. (Procko and his colleagues were not involved in the design of the Apeiron decoy.)
Apeiron developed the existing decoy following the SARS epidemic as a treatment for the coronavirus, but has also tested the drug for the treatment of various lung conditions, including acute respiratory distress syndrome (ARDS) and pulmonary arterial hypertension. Based on early data, patients appear to tolerate the treatment well, without significant side effects. Although the Apeiron product is different from the decoy that Procko and his colleagues developed, the early results are encouraging, Procko said. “We know you can inject [the Apeiron decoy] in humans and it does not hurt them, “which gives hope for their mutated ACE2 decoy, Procko said.
The Procko team has begun testing their decoy in mice infected with COVID-19 and has “not yet observed any toxicity,” he noted.
Originally published on Live Science.