[ad_1]
The groundbreaking work that was carried out in the face of the urgency of the epidemic and a wave of critically ill patients in a very short period of time.
This is the origin of the intensive care units and mechanical ventilation machines, which are now available in hospitals around the world and which play a key role in the treatment of covid-19.
It seems to be happening these days with new coronavirus,
But in August 1952, it was another disease, killed by respiratory failure to thousands of patients: polio.
Despite the fact that at that time there were 500 beds, doctors and nurses hourThe Copenhagen Blubdberma Hospital was overloaded and they could not help.
Patients were mostly young children.

polio is serious viral infection that there is no cure.
Many people go through this without symptoms.
In a small number of cases the virus affects the nerves spine and base of the brain.
this may cause paralysisusually on the feet.
But if respiratory muscles this paralysis affects a disease that can be fatal, ”explains the UK Health Service.
In the middle of the last century, Copenhagen was the epicenter of one of the worst polio epidemics what the world saw.

“50 infected people were admitted to Blebedma’s hospital every day, and 6-12 of them developed respiratory failure every day,” the magazine said in an article. nature,
“In the first weeks of the epidemic murihe87% of people with bulb poliomyelitis or bulbospinal, in which the virus attacks the brain stem or nerves that control breathing. About half were children, “he explains.
But the doctor changed the course of the situation and modern medicine: Björn Aage Ibsen, Danish anesthetist who developed part of his career in Boston, United States.
His way to deal with the Danish health care crisis, with the help of respirators and specialized personnel, has saved countless lives.
Why are intensive care units so important?
“They are important because patients who are at risk or with organ failure need careful monitoring of many parameters, with regular treatment adjustmentDoctor Philippe Jent, one of those responsible for planning coronavirus treatment at the largest hospital in Switzerland, explains the BBC.

All this special care is only possible in the intensive care unit, where the ratio of doctors and nurses per patient is higher and where specialization is very high, says Gent.
Hence it is also known as intensive medicine.
But the key to these devices lies not only in special precautions for insulation and cleaning, car availability for kidney, heart, or respiratory failure.
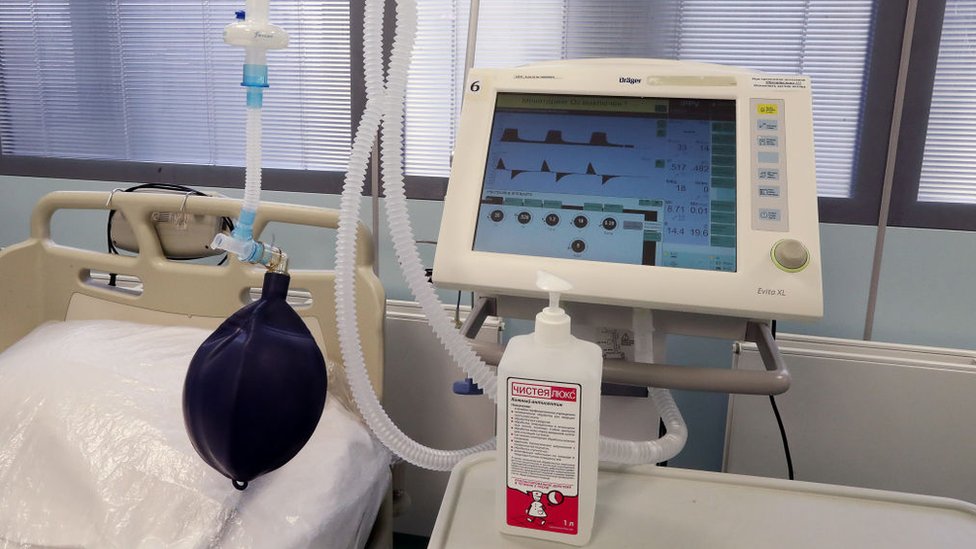
“One of the organs that often needs support is the respiratory system, that is, the lungs. Therefore, many ICU patients mechanically ventilated with respirators“He says.
Iron Respirators
But when polio hit Denmark, there was only one in the capital iron respirator or “drunk respirator” and 6 external respirators.
“Of course, this equipment was completely inadequate when the epidemic broke out,” says Alexander Lassen, head of the hospital, Henry Kai, in a 1953 scientific publication.
“We had to improviseand find ways to avoid an impossible choice situation which patient to treat on existing respirators and which patient not to treat“He said, explaining the moral dilemma that repeats today in the coronavirus pandemic.
Invented in 1928 iron respirator this requires that the human body be placed in a capsule, which creates a vacuum around the body.
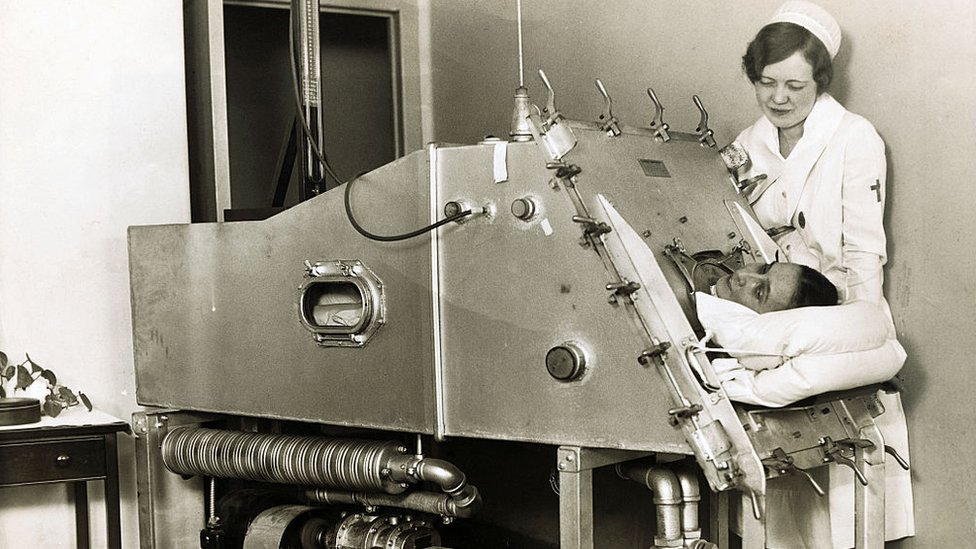
This causes the ribs and therefore the lungs to expand, letting in air.
Complications have come when a person was unconscious and he could not swallow his own saliva or stomach contents, which often entered the lungs, causing suffocation.
Designed by Danish Björn Aage Ibsen for the Blabezdma hospital, the system that solved it.
Her first patient to receive a new treatment was A 12 year old girl named Vivi.
He was dying of paralysis caused by the polio virus.
“Everyone expected him to die,” said Preben Bertelsen, a Danish anesthetist who interviewed Ibsen about this incident.
“He suggested a radical change in standard treatment, suggesting that patients with polio can be treated in the same way as surgical patients,” he added.

His idea was to inject air directly into the lungs expand them, and then allow the body to relax and exhale on its own.
He also suggested use of tracheostomy,
This is a cut in the neck through which a rubber tube is inserted that carries oxygen to the lungs.
This procedure was often used briefly during operations, but was rarely used in a hospital room.
The head physician of the hospital did not believe that the system would work, but the situation was so desperate that he decided to give it a try.
And with its Ibsen system managed to keep the girl alive,
The problem was that the method of introducing air into the rubber tube it was a guide
The medical staff had to tighten a kind of laboratory pen or bag to force air into,
Therefore, Lassen gathered as many troops as he could, and organized them in shifts.
“Now we were able to treat all patients who needed respiratory care,” said the head doctor of the hospital.
Mortality from polio with respiratory failure decreased from 87% to 31%.
At the height of the epidemic, medical staff were constantly at work between 35 and 40.
“We had around 600 trained nurses and 250 students medicine that came daily, working on a relay, “he said.
This meant that for several hours, all patients with polio collected in the same room were Toilets that systematically squeezed a piece of rubber to support them.
the rhythm must be constant, Just like observation.
A lack or malfunction in the system can lead to the death of the patient.

It was then that the doctors realized that the specialization of the staff, the organization of patients in certain departments and observation were key to the recovery of patients.
The following year, the first intensive care unit was created at the Blessedm hospital, which will be distributed throughout the rest of the world.
IN Covid-19 pandemic ICU beds and fans they continue to be a headache for governments that lack funds to care for all patients who need this type of care.
However, few people know that it was the Danish anesthetist who led to this medical progress.

Visit our special coverage
YOU MAY INTERESTED
[ad_2]