
When the number of people sent to the hospital with COVID-19 began to creep into Los Angeles County earlier this summer, officials warned that a large increase in deaths was inevitable. A record-breaking number of cases could result in a record-breaking number of deaths, they predict.
But almost two months later, that has not materialized. The coronavirus continues to kill hundreds of people every week in LA County, but the death toll has remained lower than expected.
The trend is partly due to younger people falling ill, as well as better control over the spread of the disease in high-risk institutions, such as nursing homes. But doctors say there is another factor that gives it survival rates: better treatments.
“It was so grim at first, ”said Dr. Armand Dorian, an ER doctor and chief medical officer for Verdugo Hills Hospital at USC. “Now we actually have regimens of treatments that help. … Since the beginning, say, February so far, we have learned a lot. “
The trends are not limited to LA County. In California, 3.6% of people diagnosed with COVID-19 died of the disease between March and May. Among those diagnosed between June 1 and August 3, that figure dropped to 1.2%, according to a Times analysis of state data. Extensive testing, changing demographics of patients and better patient care all play a role in that drip, experts say.
The statistic is what epidemiologists call the numerical mortality rate: the number of deaths divided by the number of cases. This measures how deadly the disease is once humans catch it – the chance of survival. While the pandemic remains bleak, the reduced rate of deaths is a glimmer of progress, experts say.
The case-mortality rate exists alongside another statistic: the mortality rate – deaths distributed by the total population – which reflects the spread of the disease within the population.
In an interview with Axios last week, President Trump reduced the “mortality rate of the nation, which is worse than most other countries,” while praising its case-mortality rate, which is better than most countries. .
But an improved rate of deaths could not compensate for the deadly spread of the deadly virus, experts say. California’s death rate has risen as the state of COVID-19’s deaths exceeded 10,000 on Thursday. If many people continue to fall ill, many people will die, even with improvements in survival rates.
Dr Tim Brewer, a specialist in infectious disease and epidemiologists at UCLA, said that even the medical improvements could be ignored as the number of patients continues to grow. An overwhelming health care system could require the ability of doctors to provide emergency care, he said.
“We have received an enormous amount of information over the last seven months, which has been useful. We just have to acknowledge to everyone that the virus is not gone, “Brewer said.
When COVID-19 patients first began seeing in hospitals in the spring, doctors did not know which medications or treatments would be effective. Little was understood about how the virus was transmitted as the best way to protect personnel. Dorian of USC described health care workers dealing with that unusual crisis as “hearts in headlights.”
But that has changed rapidly as doctors around the world study and treat the coronavirus. Research results in one country may become clinical guidelines in another within days.
“The collaboration between physicians around the world on how to best treat COVID-19 has been quite exceptional,” said Dr. Bilal Naseer, a critical care physician in Sacramento with CommonSpirit Health, a major nonprofit hospital system. “I think the level of trust of doctors and healthcare teams is now very high – how to identify patients with COVID-19 early and how to prevent serious illness is really much better understood.”
Early in the outbreak, panicked health workers administered multiple medications to patients to try to save them, not sure what might help. But that strategy made it difficult to tell what worked and did not work, so doctors did not want knowledge they could use to help the following patients.
“Doctors around the world and in LA basically threw everything we could at these patients,” Brewer said. “We had to lower our panic level a bit and do research, and do trials and studies.”
One of those studies, conducted by British scientists, led to a surprising finding. For other deadly coronaviruses, such as SARS and MERS, steroid medications have been shown to aggravate symptoms.
But UK researchers found that dexamethasone, a common low-cost steroid, reduced mortality for patients on ventilators by a third, and by a fifth for those in need of oxygen, according to the study published in June.
Doctors had already begun administering remdesivir, an antiviral medication developed by Gilead Sciences, which was shown to shorten the time it takes for patients to recover from the infection. Both drugs are now regularly prescribed by doctors who treat COVID-19 patients, they say.
“We are miles away from having real cures like vaccinations and more specific medications,” Dorian said. ‘But we have something. It feels good to say, ‘Why do not we give brake brake?’ ”
San Diego State University epidemiologist Eyal Oren pointed out that many people who become ill may not die, but will still have long-term health consequences. He warned that looking at small improvements in survival rates could dispel the reality that thousands continue to die from COVID-19, especially people of color.
“Why have we had so many cases and so many deaths?” he said. “What’s the big picture?”
But for some, the improved survival rates are a sliver of hope.
Before the last wave of patients were in LA County, most people had ever been hospitalized with COVID-19 in the province at one time just over 1,950 in late April. That record was broken in July, when more than 2,200 people were hospitalized with the infection.
Yet the average deaths were never more than what they had achieved in the spring. The provincial death toll from COVID-19 has dropped from 4% in May to 2% now, according to provincial data.
“For me, that probably means we do better care,” Dr. Jeffrey Gunzenhauser told the LA County Department of Public Health.
Gunzenhauser said the decline is likely also due to changes in who falls ill. Infections have fallen in nursing homes, whose residents are particularly vulnerable to the virus, while cases have increased among young people, who are healthier and more likely to survive, he said.
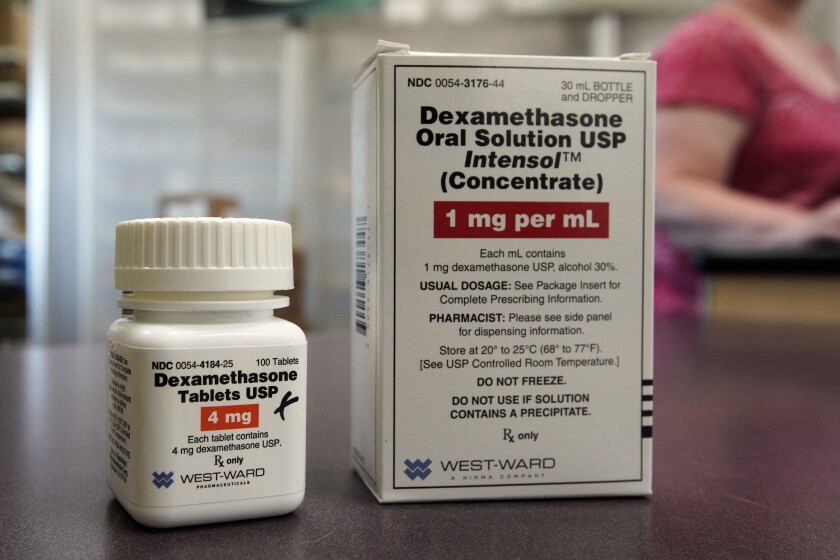
Dexamethasone is an inexpensive, widely available steroid that reduces deaths among seriously ill, hospitalized COVID-19 patients.
(United Press)
When patients end up in the hospital, doctors have new protocols to improve their chances of survival. Somewhere in the pandemic, doctors advised to put patients on ventilators as they struggled to breathe.
But now it has become clear that it may not be necessary to intubate these patients, which may open them up to other complications that actually reduce their chances of survival.
Now, doctors put patients on their stomachs to let more oxygen into their lungs and give them oxygen through tubes inserted into their noses. Patients are being put on ventilators as a last resort, doctors say.
“We were sitting on a hair trigger to put people on ventilators at the beginning of the epidemic,” said Bradley Pollock, chair of the UC Davis Department of Public Health Sciences. “If anyone sees that they are declining, we will immediately put them on a vent – that was a mistake, in retrospect.”
Doctors have also learned that COVID-19 tends to deepen patients’ blood and form blood clots, which can cause stroke and heart attacks. In some American hospitals, once faster became the cause of 40% of COVID deaths. Now doctors know how to administer anti-coagulants to prevent these deaths.
The knowledge gained over the last few months has improved care simply by building staff trust, Dorian said. Patients benefit if health care professionals do not stress and can take their time with them and listen to their needs, he said.
‘That turns people around. It’s not just medicine, ‘he said.